What is Marfan syndrome?
Marfan syndrome, a genetic disorder affecting connective tissues, paints a fascinating portrait of human biology. It’s characterized by a myriad of symptoms, many related to the skeletal system, but impacting the cardiovascular, ocular, and pulmonary systems as well. Understanding its genetic underpinnings, recognizing its diverse manifestations, and navigating its diagnostic journey is essential for managing this complex condition.
Table of Contents
Unraveling the Genetic Blueprint

Marfan syndrome is inherited in an autosomal dominant pattern. This means a single copy of the mutated gene is sufficient to cause the disorder, and there’s a 50% chance of an affected parent passing it on to their child. The culprit gene is FBN1, located on chromosome 15, responsible for producing fibrillin-1, a crucial protein for building connective tissue.
Mutations in FBN1 lead to the production of faulty fibrillin-1, disrupting the structural integrity of connective tissue throughout the body. These weakened tissues become prone to stretching, bulging, and even rupture, giving rise to the diverse symptoms of Marfan syndrome.
A Spectrum of Symptoms
Marfan syndrome exhibits a wide range of symptoms, often manifesting in unique combinations. Some common features include:
Skeletal System
Tall Stature: Individuals with Marfan syndrome are typically very tall, with long limbs, fingers, and toes.
Arachnodactyly: This refers to “spider-like” fingers, with long, slender digits.
Pectus excavatum: A sunken chest, also known as a “funnel chest.”
Scoliosis: A sideways curvature of the spine.
Kyphosis: A forward curvature of the spine, leading to a hunchback appearance.
Cardiovascular System

Aortic Aneurysm: A widening of the aorta, the main artery carrying blood from the heart, increasing the risk of rupture.
Mitral Valve Prolapse: A condition where the mitral valve, separating the heart’s upper and lower chambers, doesn’t close properly, potentially causing a heart murmur.
Ocular System
Lens Dislocation: The lens of the eye can become displaced, affecting vision.
Myopia: Nearsightedness.
Retinal Detachment: A separation of the retina from the back of the eye, potentially leading to vision loss.
Pulmonary System
Pneumothorax: Collapsed lung, often due to the weakened connective tissue in the lungs.
Spontaneous Pneumothorax: A collapsed lung without any obvious cause.
Decoding the Clues: Diagnosis
Diagnosing Marfan syndrome relies on a combination of clinical evaluation, genetic testing, and imaging studies:
Clinical Evaluation
A physician will assess the patient’s medical history, family history, and physical characteristics. Specific features like tall stature, arachnodactyly, and heart murmurs are important indicators.
Genetic Testing
Analysis of the FBN1 gene can confirm the presence of mutations associated with Marfan syndrome.
Imaging Studies
Echocardiogram: Examines the heart’s structure and function, particularly focusing on the aorta.
Chest X-ray: Identifies skeletal abnormalities like scoliosis and pectus excavatum.
MRI (Magnetic Resonance Imaging): Provides detailed images of the heart, aorta, and other organs.
Navigating the Treatment Path
Treatment for Marfan syndrome is tailored to address the specific symptoms and complications experienced by each individual. While there’s no cure for the underlying genetic condition, management focuses on preventing and mitigating potential complications:
Cardiovascular Management
Regular Monitoring: Frequent echocardiograms are crucial to track aortic size and function.
Beta-blockers: Medications that slow the heart rate and reduce stress on the aorta.
Surgery: Aortic aneurysm repair may be necessary if the aorta widens significantly.
Skeletal Management
Bracing: May be used to correct spinal curvature.
Physical Therapy: Strengthens muscles and improves posture.
Surgery: In cases of severe spinal deformities.
Ocular Management
Eye Exams: Regular eye examinations are essential to monitor for lens dislocation and other eye problems.
Laser Surgery: May be used to correct lens dislocation.
Surgery: May be necessary for retinal detachment.
Pulmonary Management
Oxygen Therapy: May be required for pneumothorax.
Surgery: In cases of severe pneumothorax.
Living with Marfan Syndrome
Living with Marfan syndrome requires a proactive approach. Individuals with the condition should be closely monitored by medical professionals, particularly for cardiovascular complications. Regular checkups, adherence to prescribed medication, and lifestyle modifications are crucial for managing the disorder effectively.
Support and Resources
For individuals with Marfan syndrome and their families, accessing support and resources is vital. Organizations like the Marfan Foundation provide valuable information, connect individuals with medical experts, and offer support groups and educational materials.
Conclusion
Marfan syndrome, while a complex condition, doesn’t define a person’s life. Early diagnosis, ongoing monitoring, and effective management can significantly improve quality of life and ensure a healthier future. By understanding the genetics, symptoms, diagnosis, and treatment of Marfan syndrome, individuals can embrace a fulfilling life while navigating the complexities of this genetic disorder.
Frequently Asked Questions(FAQ)
What is Genetic Blueprint?
A Finnish business called Blueprint Genetics specializes in bioinformatics and customized genomic testing. Since its founding in 2011, the business has grown to become a major force in the global genetic testing industry.
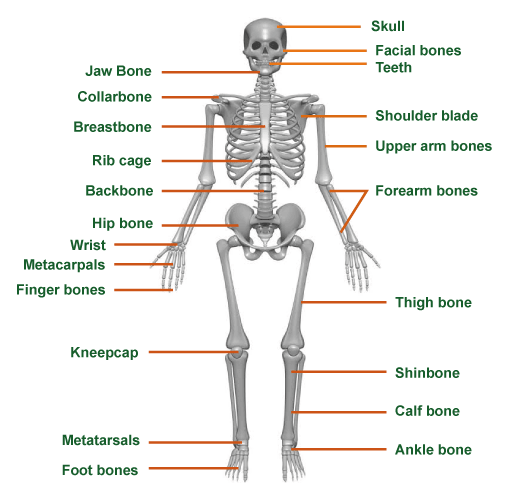
Define the term skeletal system?
The structural support system of your body is the skeletal system. It creates blood cells, gives your body form, permits movement, shields your organs, and stores minerals. The musculoskeletal system is another name for the skeletal system.
Related Articles