What is Candida glabrata?
Candida glabrata is a type of yeast (a fungus) that naturally lives in our body, especially in areas like the mouth, intestines, and urinary tract. In most healthy people, it doesn’t cause any problems. But when someone’s immune system is weak like during cancer treatment, after an organ transplant, or if they have HIV/AIDS this yeast can grow too much and cause infections.
Summary of Candida glabrata
- Candida glabrata is a yeast-like fungus that normally lives in the human body but can cause serious infections, especially in people with weak immune systems.
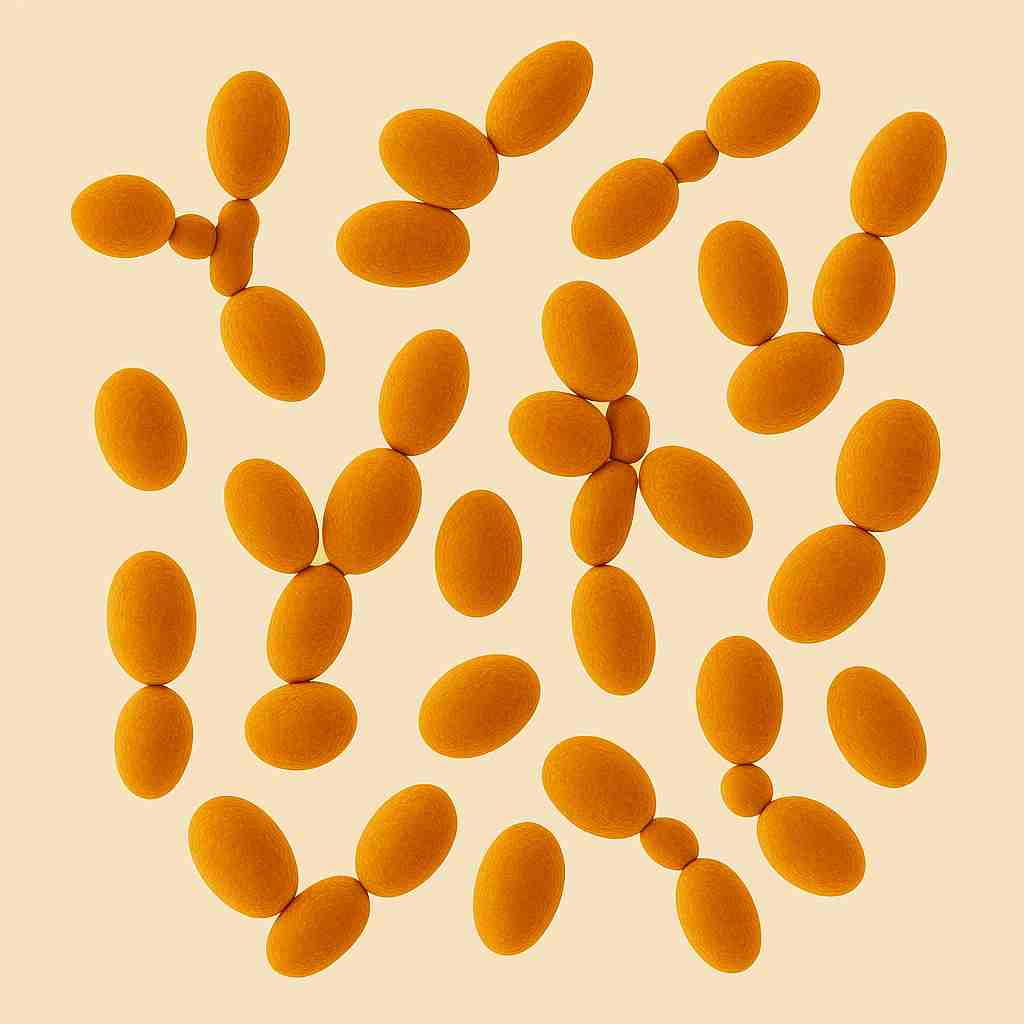
- Unlike Candida albicans, it does not form true hyphae but is still highly resistant to many antifungal drugs.
- Its rising drug resistance and ability to survive inside host cells make it a growing concern in modern healthcare.
Table of Contents
Biological Characteristics of C. glabrata
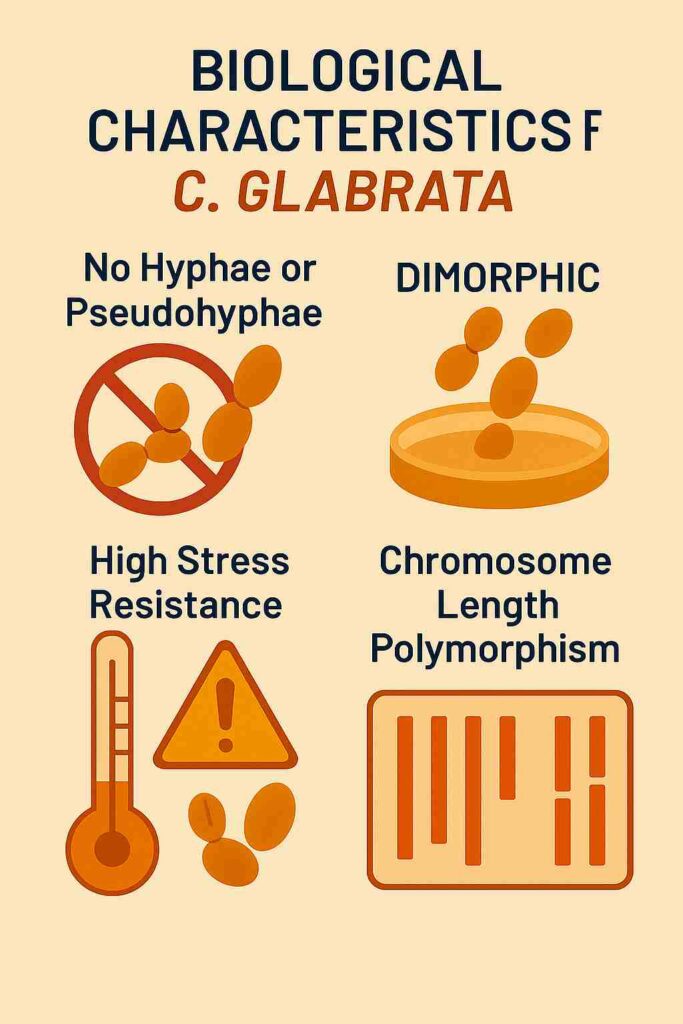
Unlike its cousin Candida albicans, C. glabrata does not form hyphae or pseudohyphae, existing predominantly in a yeast form. This morphological distinction contributes to its unique pathogenic profile and challenges in clinical management. Its genome exhibits remarkable plasticity, allowing rapid adaptation to environmental stresses, including antifungal exposure. This adaptability is facilitated by mechanisms such as chromosomal rearrangements and gene amplification, enhancing its survival in hostile conditions.
Virulence Factors of C. glabrata
Despite lacking traditional virulence traits like hyphal formation, C. glabrata employs several strategies to establish infection:
- Adhesion: The expression of epithelial adhesin (EPA) genes enables the yeast to adhere to host tissues and medical devices.
- Biofilm Formation: C. glabrata can form robust biofilms on surfaces, providing protection against antifungal agents and the host immune system.
- Enzymatic Activity: The production of enzymes such as proteases and phospholipases facilitates tissue invasion and nutrient acquisition, contributing to pathogenicity.
Antifungal Resistance of Candida glabrata

C. glabrata exhibits notable resistance to multiple antifungal classes:
- Azoles: Intrinsic resistance to azoles, particularly fluconazole, is common, often due to overexpression of drug efflux pumps and mutations in target enzymes.
- Echinocandins: Resistance can develop through mutations in FKS genes, which encode components of the β-1,3-glucan synthase complex, a target of echinocandins.
- Polyenes: While generally effective, resistance to polyenes like amphotericin B has been reported, though less frequently than with other antifungal classes.
This multidrug resistance complicates treatment and underscores the need for susceptibility testing and novel therapeutic approaches.
Clinical Manifestations of Candida glabrata
C. glabrata can cause a range of infections, including:
- Urinary Tract Infections (UTIs): Particularly in hospitalized or catheterized patients.
- Vulvovaginal Candidiasis: Especially in women with recurrent infections or those who have used antibiotics.
- Candidemia: A bloodstream infection that can lead to systemic involvement, particularly in immunocompromised individuals.
These infections are often associated with high morbidity and mortality, especially when caused by resistant strains.
Treatment Strategies of Candida glabrata
Management of C. glabrata infections requires a nuanced approach:
- Echinocandins: Often considered first-line therapy due to their efficacy against C. glabrata.
- Amphotericin B: Used in cases where resistance to other antifungals is present, despite its potential toxicity.
- Flucytosine: May be used in combination therapies to enhance efficacy.
Given the potential for resistance, antifungal susceptibility testing is crucial to guide effective treatment.
Conclusion
Candida glabrata has transitioned from a benign commensal organism to a formidable pathogen, particularly in healthcare settings. Its ability to resist multiple antifungal agents and cause severe infections underscores the need for vigilant surveillance, prompt diagnosis, and tailored treatment strategies. Ongoing research into its pathogenic mechanisms and resistance patterns is essential to develop effective interventions and improve patient outcomes.
Frequently Asked Questions (FAQs)
How does Candida glabrata differ from Candida albicans?
Unlike Candida albicans, which can form hyphae (long, branching structures), C. glabrata remains in a yeast form and does not produce hyphae. Additionally, C. glabrata tends to be more resistant to certain antifungal medications, making infections harder to treat.
What types of infections can Candida glabrata cause?
C. glabrata can lead to various infections, including urinary tract infections (UTIs), bloodstream infections (candidemia), and mucosal infections like oral thrush and vaginal yeast infections. In severe cases, it can cause systemic infections affecting multiple organs.
How are Candida glabrata infections treated?
Treatment typically involves antifungal medications. However, C. glabrata often shows resistance to common antifungals like fluconazole. Therefore, doctors may prescribe alternative treatments such as echinocandins or amphotericin B, depending on the infection’s severity and location.
Related Articles