What do you mean by Fluconazole?
Fluconazole, a widely used antifungal medication, has revolutionized the treatment of fungal infections. Its versatility, effectiveness, and relatively low side-effect profile make it a cornerstone of antifungal therapy. Let’s delve into the intricacies of fluconazole, from its mechanism of action to its clinical applications.
Table of Contents
Mechanism of Action: Targeting the Fungal Engine
Its potent antifungal action lies in its ability to inhibit an essential fungal enzyme, cytochrome P450 14α-demethylase (CYP450 14α-demethylase). This enzyme is crucial for the synthesis of ergosterol, a vital component of fungal cell membranes. Ergosterol provides structural integrity and regulates membrane permeability, ensuring the smooth functioning of the fungal cell.
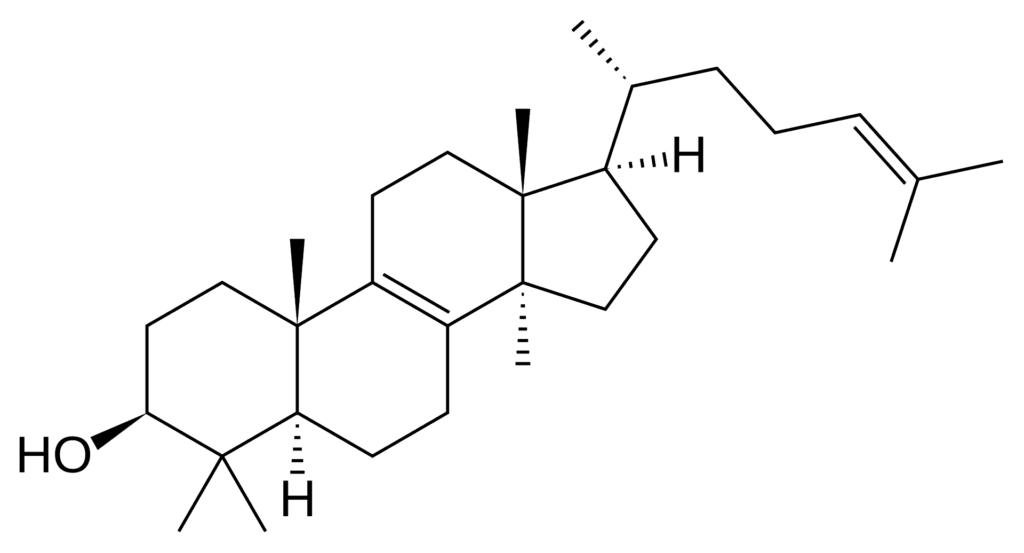
By blocking CYP450 14α-demethylase, it prevents ergosterol production, leading to accumulation of toxic sterol precursors within the fungal cell. This disruption of membrane integrity disrupts fungal growth and eventually leads to cell death.
Spectrum of Activity: A Wide Range of Targets
Its effectiveness extends to a broad spectrum of fungal infections, encompassing both superficial and systemic fungal infections. This wide-ranging activity makes its a versatile and valuable therapeutic option.
Superficial fungal infections
It effectively treats superficial infections like candidiasis (yeast infections) affecting the skin, mucous membranes, and nails. This includes conditions like oral thrush (candidiasis in the mouth), vaginal candidiasis, and cutaneous candidiasis.
Systemic fungal infections
It is also highly effective against systemic fungal infections, which can affect internal organs and spread throughout the body. It is commonly used to manage cryptococcal meningitis, a severe fungal infection of the brain and spinal cord, and coccidioidomycosis, a respiratory fungal infection.
Prophylactic use
It can also be used prophylactically to prevent fungal infections in high-risk individuals, such as those undergoing bone marrow transplantation or those with weakened immune systems due to conditions like AIDS or cancer chemotherapy.
Resistance: A Challenge to Overcome
While it offers significant therapeutic benefits, the emergence of resistance poses a challenge. Some fungal species, particularly Candida albicans, have developed resistance mechanisms to fluconazole, limiting its effectiveness.
Mechanisms of resistance:
Mutations in the CYP450 14α-demethylase gene
Mutations in this gene can lead to a decrease in the enzyme’s affinity for fluconazole, reducing its ability to bind and inhibit the enzyme.
Increased efflux pumps
Fungal cells can increase the expression of efflux pumps, which actively pump fluconazole out of the cell, reducing its intracellular concentration.
Pharmacokinetics: The Journey of Fluconazole in the Body
It exhibits favorable pharmacokinetic properties, contributing to its clinical success.
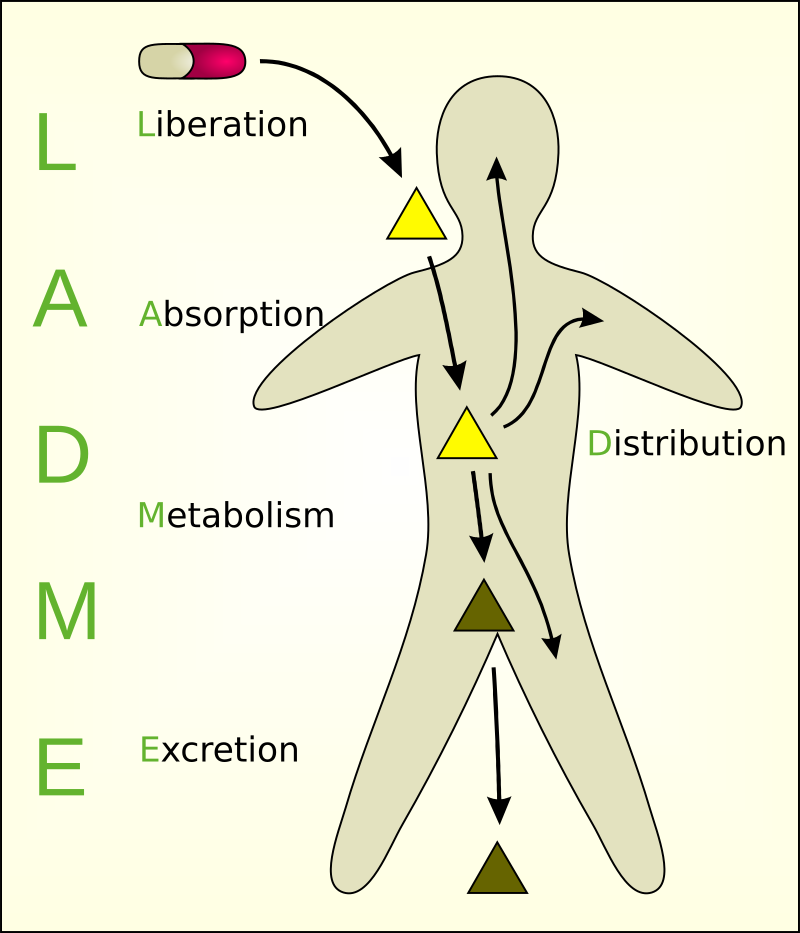
Absorption: It is well absorbed after oral administration, reaching peak plasma concentrations within 2-4 hours.
Distribution: It readildyistributes to various tissues and organs, including the brain, cerebrospinal fluid (CSF), and skin.
Metabolism: It undergoes minimal metabolism, primarily excreted unchanged in the urine.
Half-life: It has a long half-life, ranging from 20-30 hours, allowing for once-daily dosing and sustained therapeutic concentrations.
Clinical Uses: A Versatile Weapon Against Fungi
Fluconazole’s broad-spectrum activity and favorable pharmacokinetics have made it a cornerstone of antifungal therapy for a diverse range of fungal infections.
Candidiasis
It is a first-line treatment for candidiasis affecting various sites, including oral thrush, vaginal candidiasis, esophageal candidiasis, and cutaneous candidiasis.
Cryptococcal meningitis
It is the drug of choice for cryptococcal meningitis, offering excellent efficacy and a long half-life, making it suitable for long-term maintenance therapy.
Coccidioidomycosis
Fluconazole is an effective treatment option for coccidioidomycosis, particularly in patients with mild or moderate disease.
Prophylaxis
Fluconazole is frequently used for fungal prophylaxis in high-risk individuals, such as those undergoing bone marrow transplantation or receiving immunosuppressive therapy.
Other fungal infections
Fluconazole is also employed for various other fungal infections, including aspergillosis, blastomycosis, and histoplasmosis.
Side Effects: A Relatively Safe Profile
Fluconazole generally has a favorable safety profile, with side effects being relatively infrequent and mild. However, some potential side effects may occur.
Gastrointestinal disturbances: Nausea, vomiting, and abdominal pain are among the most common side effects.
Hepatotoxicity: Fluconazole can cause liver damage, particularly in individuals with pre-existing liver disease or those taking multiple medications.
Skin reactions: Rash, itching, and hives may occur, and in rare cases, fluconazole can trigger Stevens-Johnson syndrome, a serious skin reaction.
Drug interactions: Fluconazole can interact with several medications, potentially affecting their effectiveness or increasing the risk of side effects.
Conclusion: A Powerhouse in the Fight Against Fungal Infections
Fluconazole stands as a powerful antifungal agent, offering a broad spectrum of activity, favorable pharmacokinetics, and a relatively safe profile. Its ability to target a vital fungal enzyme, combined with its long half-life and good tissue penetration, has made it a valuable tool for treating a wide range of fungal infections. While resistance poses a challenge, ongoing research and innovative approaches are continuously expanding our arsenal against these fungal foes. Understanding fluconazole’s mechanism of action, spectrum of activity, pharmacokinetics, and potential side effects is crucial for optimizing its use and ensuring safe and effective treatment of fungal infections.
Frequently Asked Questions(FAQ)
What do you mean by efflux pumps?
Efflux pumps control who enters and leaves a space, much like the bouncers in a cell nightclub. These are transmembrane proteins that actively move substances out of the cell, including poisons, medications, and even necessary nutrients.
What do you mean by Coccidioidomycosis?
Often referred to as “Valley Fever,” coccidioidomycosis (kok-si-di-oy-doh-my-ko-sis) is a lung infection brought on by a fungus that thrives in some regions’ soil, mostly in the Southwestern region of the United States.
Related Articles