Aminoglycosides are a class of antibiotics that have been widely used since the 1940s to combat serious bacterial infections, particularly those caused by Gram-negative bacteria. Examples of these antibiotics include gentamicin, streptomycin, and amikacin, which are frequently employed in treating conditions like sepsis, urinary tract infections (UTIs), and pneumonia.
Table of Contents
Antimicrobial Activity
Aminoglycosides are effective at killing bacteria, especially aerobic Gram-negative types, including problematic pathogens such as Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, and Enterobacter species. Although they are less effective on their own against Gram-positive bacteria, when combined with antibiotics like beta-lactams, It can target difficult Gram-positive organisms such as Staphylococcus aureus and Enterococcus species.
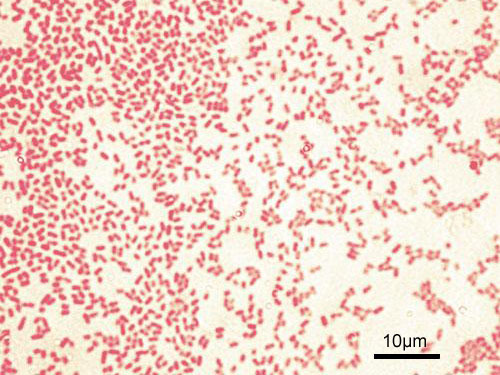
Their ability to combat infections caused by resistant bacteria makes them particularly useful in hospitals. However, aminoglycoside are ineffective against anaerobic bacteria, fungi, and viruses, limiting their use to specific bacterial infections.
Mode of Action
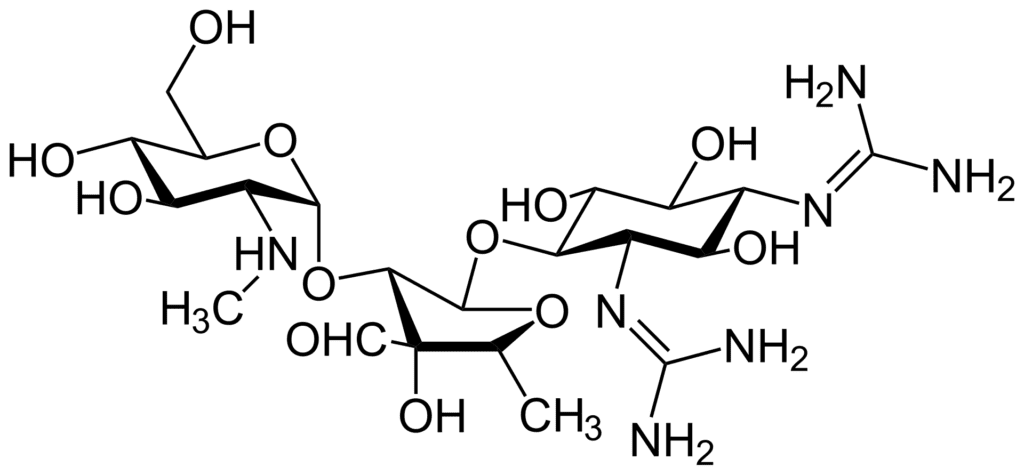
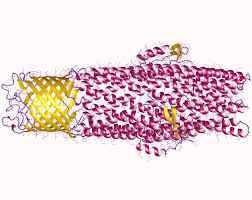
Aminoglycoside work by disrupting protein synthesis within bacterial cells. They bind to the 30S subunit of the bacterial ribosome, which prevents the accurate translation of genetic material into proteins. This leads to the production of faulty or harmful proteins that eventually kill the bacteria. Additionally, they damage the bacterial cell membrane, increasing permeability and enhancing their bactericidal effect. Their rapid action makes them invaluable for treating life-threatening infections.
Mechanisms of Resistance
Over time, bacteria have developed various ways to resist the effects of aminoglycoside:
Enzymatic Modification
Some bacteria produce enzymes that modify aminoglycoside, neutralizing their effectiveness. These enzymes (called aminoglycoside-modifying enzymes, or AMEs) chemically alter the antibiotic’s structure, preventing it from binding to the bacterial ribosome.
Decreased Uptake
Certain bacteria change their cell membranes, limiting the amount of aminoglycoside that can enter the cell. Since these antibiotics require active transport to reach their target, any alteration in membrane permeability can lead to resistance.
Efflux Pumps
Some bacterial species use efflux pumps to push aminoglycosides out of the cell, reducing the intracellular concentration of the drug and weakening its effect.
Target Modification
Mutations in the ribosome can reduce aminoglycosides’ ability to bind, thus allowing the bacteria to continue making proteins and survive in the presence of the drug.
These resistance mechanisms pose challenges in treating infections, especially with the rise of multidrug-resistant bacteria.
Pharmacological Properties
Due to poor absorption through the gastrointestinal tract, aminoglycosides are typically administered intravenously or intramuscularly. They work through concentration-dependent killing, meaning higher doses are more effective at destroying bacteria. This property also gives them a “post-antibiotic effect,” where bacterial suppression continues even after drug levels drop.
However, aminoglycosides have a narrow therapeutic window, meaning the difference between a safe dose and a toxic one is small. This requires careful monitoring of drug levels in the blood to avoid serious side effects.
Pharmacokinetics
Aminoglycosides are primarily excreted through the kidneys, making them useful for treating urinary tract infections. However, in patients with kidney problems, the drug can accumulate, leading to toxicity. While the half-life of aminoglycosides is relatively short, dose adjustments are often needed for patients with impaired kidney function to avoid harmful buildup.
Side Effects
One of the significant drawbacks of aminoglycosides is their potential for causing toxicity, particularly in the kidneys (nephrotoxicity) and ears (ototoxicity). Nephrotoxicity involves damage to kidney cells, leading to reduced kidney function, which can sometimes be reversible. Ototoxicity, however, can result in permanent hearing loss or balance issues, as aminoglycosides affect the inner ear.
Because of these risks, aminoglycosides are generally used only for short periods and require close monitoring of kidney function and hearing during treatment.
Clinical Use
In summary, aminoglycosides are powerful antibiotics that target a wide range of Gram-negative bacteria. However, their use must be carefully managed to avoid toxicity and to address the growing issue of antibiotic resistance. Responsible prescribing and close patient monitoring are key to maintaining their effectiveness in treating bacterial infections.
Despite their toxic potential, aminoglycosides remain essential in treating severe bacterial infections, particularly those caused by drug-resistant bacteria. They are often used in combination with other antibiotics to enhance effectiveness and treat mixed infections.
Frequently Asked Questions(FAQ)
Define aminoglycosides?
Since the 1940s, aminoglycosides have been a commonly utilized class of antibiotics to treat serious bacterial infections, especially those brought on by Gram-negative bacteria.
Write the Clinical Use of Aminoglycosides?
Aminoglycosides are mostly utilized in hospital settings to treat drug-resistant bacteria and severe Gram-negative infections such as sepsis, lung infections, and urinary tract infections.
Related Articles