What is Pulmonary air volume and capacities?
Pulmonary air volume and capacities are measurements of the air that moves in and out of the lungs. They are important indicators of lung function and are often measured using a device called a spirometer. These measurements are used to diagnose and monitor respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and restrictive lung diseases. The process of respiration is essential for sustaining life.
The human respiratory system facilitates the exchange of gases oxygen and carbon dioxide between the external environment and the internal body. Central to this function is the ability of the lungs to accommodate varying volumes of air during different phases of the respiratory cycle. The measurement of pulmonary volumes and capacities is an important aspect of respiratory physiology. These parameters are used not only to understand normal pulmonary function but also to detect, diagnose, and monitor various respiratory disorders.
Summary of Pulmonary air volume
- pulmonary air volume is a key indicator of lung health, showing how effectively the lungs can hold and move air.
- Understanding these volumes helps detect breathing problems early and guide proper treatment.
- Regular monitoring can be especially important for people with respiratory conditions.
Table of Contents
Pulmonary vein
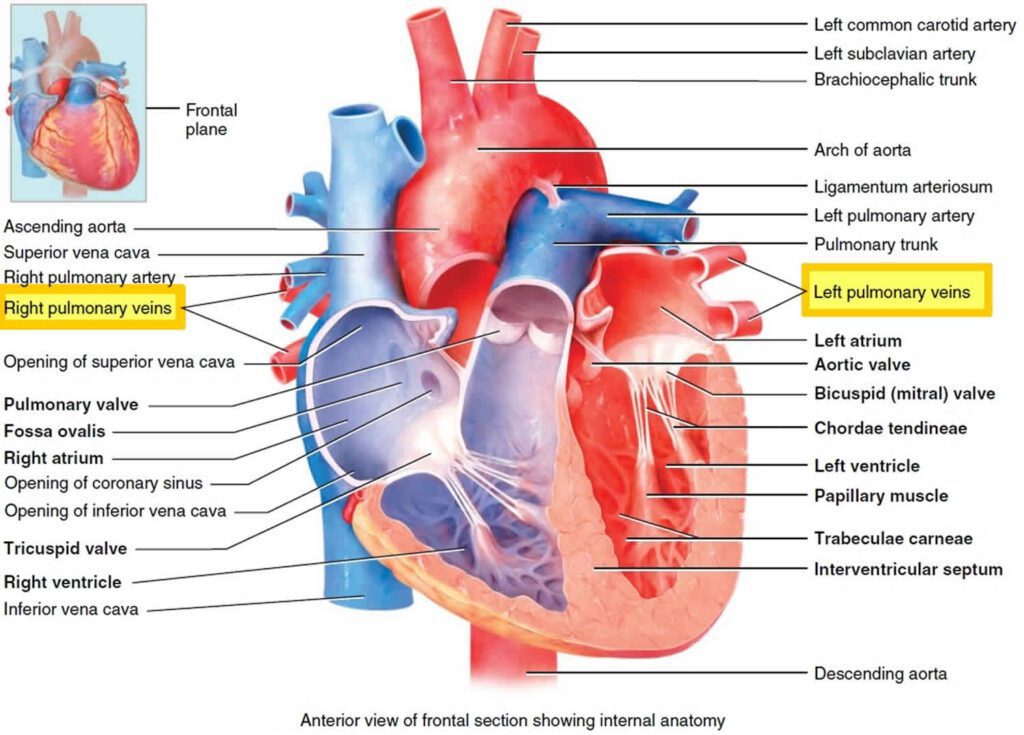
The pulmonary veins are the blood vessels that carry oxygen-rich blood from the lungs to the heart. There are four pulmonary veins, two from each lung, and they deliver the oxygenated blood into the left atrium of the heart. This blood is then pumped out to the rest of the body.
Pulmonary respiration
Pulmonary respiration is the process of breathing through the lungs. It involves inhaling oxygen from the air into the lungs and exhaling carbon dioxide out of the body. This exchange of gases takes place in the alveoli, the tiny air sacs in the lungs.
Pulmonary Air Volumes
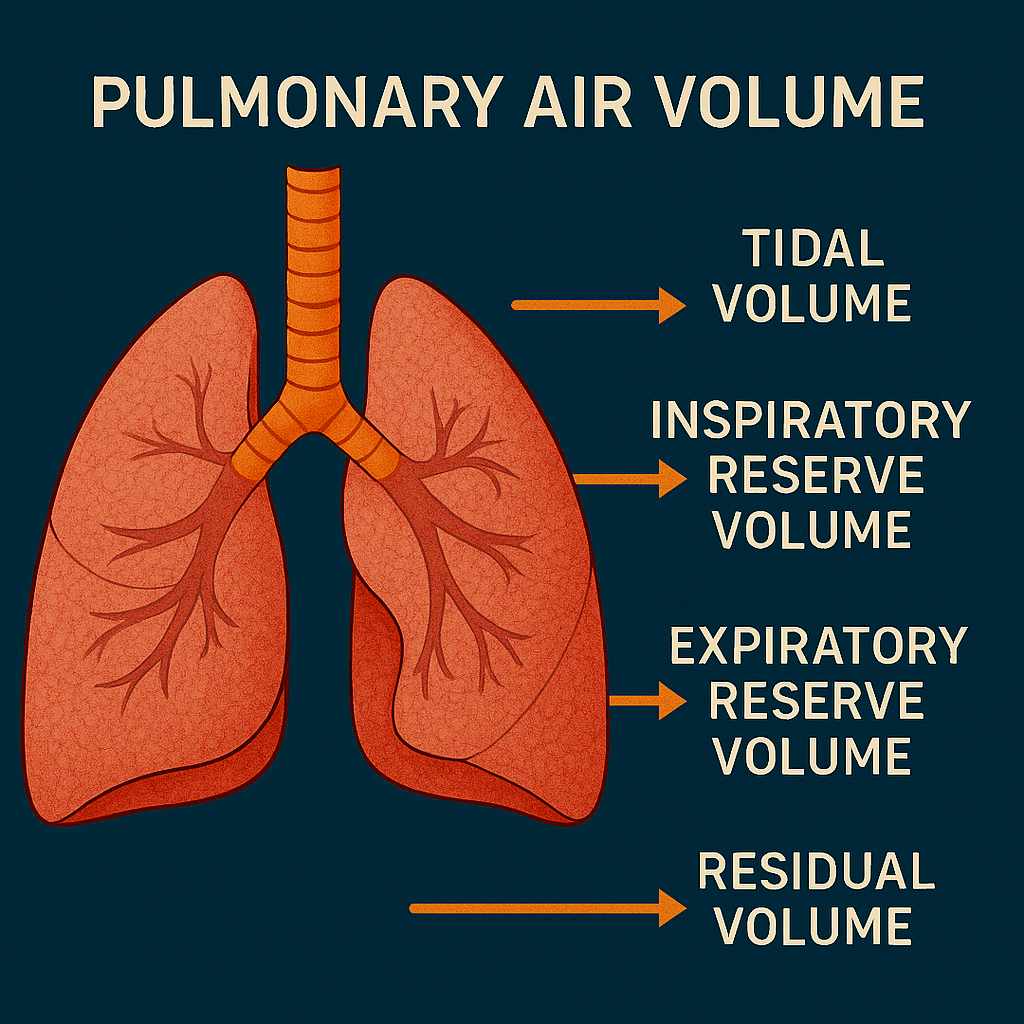
Pulmonary air volumes refer to the discrete quantities of air that can be inhaled, exhaled, or present in the lungs at any given time during the respiratory cycle. Pulmonary air volumes are measured under specific conditions and provide fundamental data regarding lung function.
1. Tidal Volume (TV)
Tidal Volume is the volume of air inhaled or exhaled in a single breath during quiet, normal breathing. It reflects the baseline respiratory effort without exertion.
- Average Value: Approximately 500 milliliters in a healthy adult.
- Physiological Role: Maintains the continuous exchange of gases at rest.
2. Inspiratory Reserve Volume (IRV)
Inspiratory Reserve Volume is the maximum volume of air that can be forcibly inhaled after a normal tidal inspiration.
- Average Value: Around 3000 to 3100 milliliters.
- Significance: Represents the capacity for increased oxygen intake during physical activity or stress.
3. Expiratory Reserve Volume (ERV)
Expiratory Reserve Volume is the maximum volume of air that can be forcibly exhaled after the end of a normal tidal expiration.
- Average Value: Approximately 1000 to 1200 milliliters.
- Function: Indicates the potential for additional air expulsion beyond passive expiration.
4. Residual Volume (RV)
Residual Volume is the amount of air remaining in the lungs after a maximal forced exhalation. This volume cannot be expelled from the lungs and is crucial in preventing alveolar collapse.
- Average Value: About 1200 milliliters.
- Importance: Ensures that gas exchange can continue even between breaths.
Pulmonary Capacities
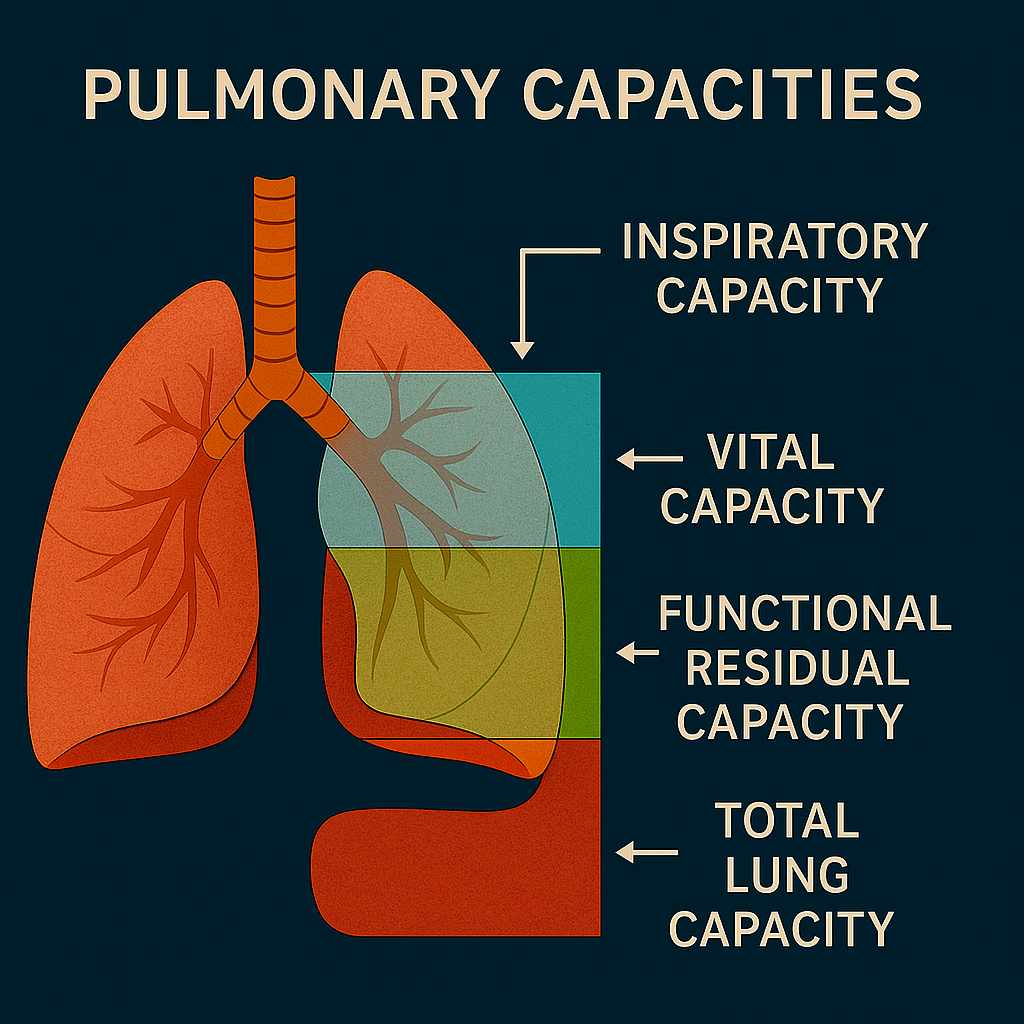
Pulmonary capacities are calculated by combining two or more of the basic pulmonary volumes. These capacities provide a more comprehensive understanding of the functional potential of the lungs.
1. Inspiratory Capacity (IC)
Inspiratory Capacity is the total volume of air that can be inhaled after a normal expiration. It is the sum of the Tidal Volume and Inspiratory Reserve Volume.
- Formula: IC = TV + IRV
- Average Value: Approximately 3500 to 3600 milliliters.
- Clinical Utility: Reflects the maximal inspiratory ability of the lungs.
2. Functional Residual Capacity (FRC)
Functional Residual Capacity is the amount of air remaining in the lungs after a normal tidal expiration. It is the sum of the Expiratory Reserve Volume and Residual Volume.
- Formula: FRC = ERV + RV
- Average Value: Around 2300 to 2400 milliliters.
- Physiological Role: Acts as a buffer to maintain continuous gas exchange during the respiratory cycle.
3. Vital Capacity (VC)
Vital Capacity is the maximum volume of air that can be exhaled following a maximum inhalation. It encompasses the Tidal Volume, Inspiratory Reserve Volume, and Expiratory Reserve Volume.
- Formula: VC = TV + IRV + ERV
- Average Value: Approximately 4500 to 4800 milliliters.
- Clinical Significance: Often used in spirometry tests to assess overall lung function.
4. Total Lung Capacity (TLC)
Total Lung Capacity is the maximum volume of air that the lungs can hold after a maximal inspiratory effort. It includes all four volumes: Tidal Volume, Inspiratory Reserve Volume, Expiratory Reserve Volume, and Residual Volume.
- Formula: TLC = TV + IRV + ERV + RV
- Average Value: Around 6000 milliliters in a healthy adult.
- Importance: Represents the full capacity of the lungs and is critical for evaluating pulmonary health.
Factors Affecting Pulmonary Air Volume and Capacities
Pulmonary volumes and capacities are influenced by several intrinsic and extrinsic factors:
- Age: Lung elasticity and chest wall compliance decrease with age, leading to reduced vital capacity.
- Sex: Males generally have larger lung volumes than females.
- Height and Body Size: Taller individuals typically have greater lung capacities.
- Physical Activity: Athletes often exhibit higher vital capacity due to enhanced respiratory muscle strength.
- Altitude: Individuals living at higher altitudes may develop larger lung volumes as an adaptation to lower oxygen levels.
Measurement of Pulmonary Air Volume and Capacities
The most common method for evaluating Pulmonary Air Volume and Capacities is spirometry, a technique that measures airflow and the volume of air entering and leaving the lungs.
Spirometry
Spirometry is a simple, non-invasive test in which a subject breathes into a mouthpiece connected to a spirometer. It records the volume and speed of air movement during inhalation and exhalation.
- Parameters Measured:
- Tidal Volume (TV)
- Expiratory Reserve Volume (ERV)
- Vital Capacity (VC)
- Forced Vital Capacity (FVC)
- Forced Expiratory Volume in 1 second (FEV1)
Note: Residual Volume (RV) and capacities involving RV (FRC, TLC) cannot be measured directly by spirometry. They require additional techniques.
Other Techniques
- Body Plethysmography: Measures lung volumes using changes in pressure within a sealed chamber.
- Helium Dilution and Nitrogen Washout: Involves inhaling a known concentration of an inert gas to estimate residual volume and functional residual capacity.
Clinical Relevance of pulmonary volumes and capacities
Assessment of pulmonary volumes and capacities is essential in the diagnosis and management of respiratory diseases. Abnormalities in these parameters help distinguish between obstructive and restrictive pulmonary conditions.
Obstructive Lung Diseases
Characterized by difficulty in exhaling air from the lungs.
- Examples: Asthma, Chronic Obstructive Pulmonary Disease (COPD), Emphysema.
- Findings:
- Increased Residual Volume (RV)
- Increased Total Lung Capacity (TLC)
- Decreased Vital Capacity (VC)
- Decreased FEV1/FVC ratio
Restrictive Lung Diseases
Involve reduced lung expansion and decreased lung volume.
- Examples: Pulmonary fibrosis, Sarcoidosis, Obesity-related hypoventilation.
- Findings:
- Decreased Tidal Volume (TV)
- Decreased Inspiratory Reserve Volume (IRV)
- Decreased Total Lung Capacity (TLC)
- Normal or increased FEV1/FVC ratio
Physiological Adaptations for pulmonary volumes and capacities
Lung volumes can be modified through training and environmental exposure:
- Exercise: Regular aerobic activity increases tidal volume and improves ventilatory efficiency.
- Yoga and Breathing Techniques: Practices like pranayama enhance voluntary control of breathing and improve inspiratory and expiratory volumes.
- High Altitude: Prolonged exposure leads to increased red blood cell production and may mildly increase vital capacity as an adaptive response.
Conclusion
Pulmonary air volumes and capacities form the cornerstone of respiratory physiology. These measurements offer crucial insight into the functional status of the lungs and are indispensable tools in both clinical and physiological assessments. Understanding these parameters allows healthcare professionals to accurately evaluate lung function, detect abnormalities, and monitor disease progression.
By studying pulmonary volumes and capacities, one gains a deeper appreciation of the intricate mechanisms that sustain life with each breath.
Frequently Asked Questions (FAQs)
What do you mean by Pulmonary vein?
The pulmonary veins are the blood vessels that carry oxygen-rich blood from the lungs to the heart. There are four pulmonary veins, two from each lung, and they deliver the oxygenated blood into the left atrium of the heart. This blood is then pumped out to the rest of the body.
Define Pulmonary respiration ?
Pulmonary respiration is the process of breathing through the lungs. It involves inhaling oxygen from the air into the lungs and exhaling carbon dioxide out of the body. This exchange of gases takes place in the alveoli, the tiny air sacs in the lungs.
What do you understand Pulmonary respiration?
Pulmonary respiration is the process of breathing, where oxygen is taken into the lungs and carbon dioxide is released. It allows the body to get the oxygen it needs for energy and remove waste gases.
Related Articles

