What is urine formation?
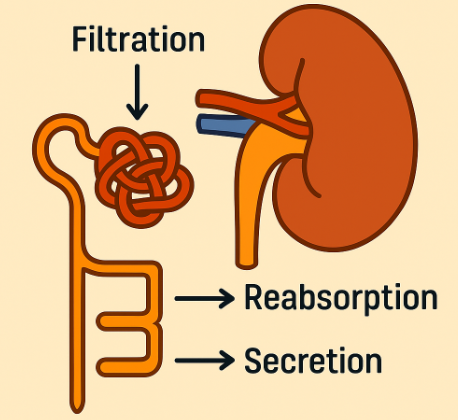
Urine formation is a vital process carried out by the kidneys to maintain the body’s internal environment. It involves filtering blood to remove waste products and excess substances, ensuring the balance of fluids and electrolytes. This process occurs in the nephrons, the functional units of the kidneys, through three main steps: glomerular filtration, tubular reabsorption, and tubular secretion.
Summary of urine formation
- Urine formation starts when your kidneys filter blood, pulling out waste and excess substances while saving what your body needs.
- Next, the kidneys fine-tune this fluid by reabsorbing water, salts, and nutrients, ensuring nothing valuable is lost.
- Finally, they add a last round of toxins and acids before sending it all out as urine keeping your body clean and balanced
Table of Contents
The Kidney’s Role: More Than Just a Filter
Before diving into urine formation, let’s understand the kidney’s structure and why it’s so crucial:
- Location: Two bean-shaped organs near the lower back.
- Function: Filter blood, remove waste, regulate blood pressure, balance electrolytes, and maintain pH.
- Key Structures:
- Nephrons (functional units where urine is made).
- Renal corpuscle (filters blood).
- Renal tubules (modify filtered fluid into urine).
There are three steps of urine formation,
- Glomerular Filtration
- Tubular Reabsorption
- Tubular Secretion
Step 1: Glomerular Filtration – The First Sieve
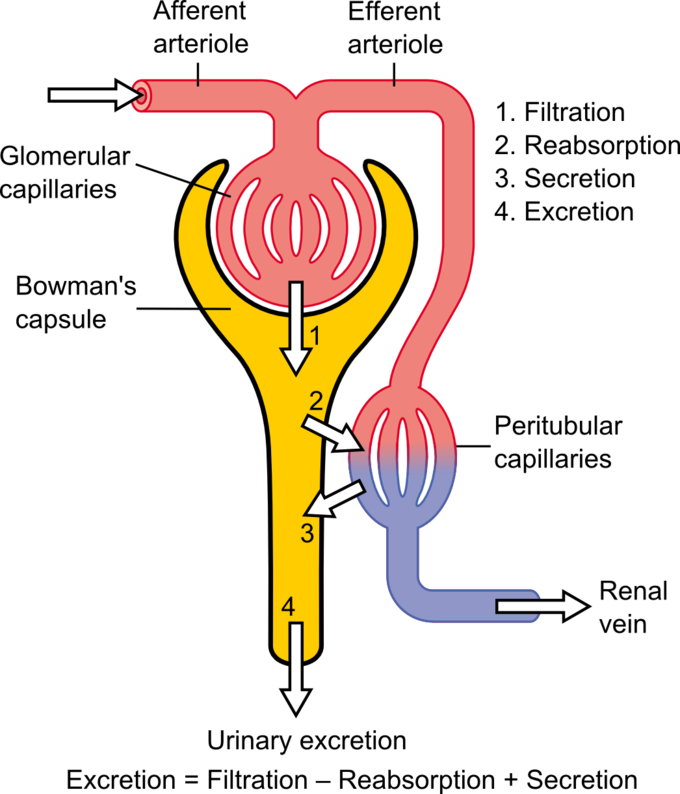
What Happens?
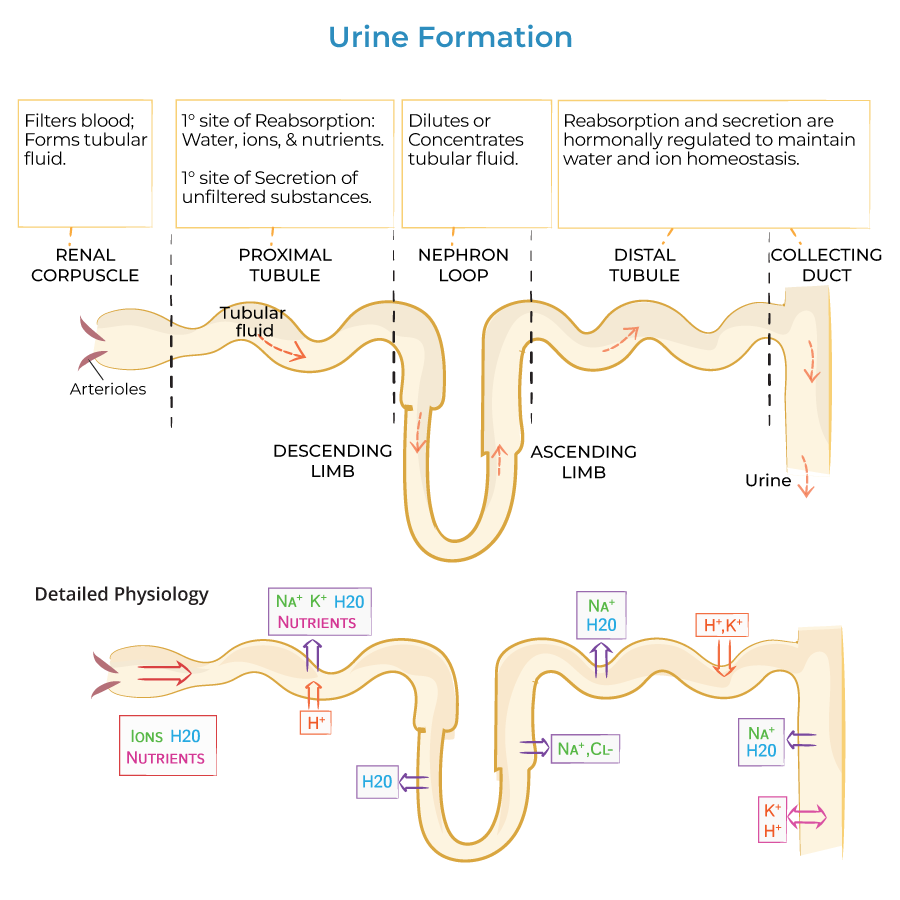
Blood enters the glomerulus (a tiny ball of capillaries) inside the nephron. Here, high pressure forces fluid out of the blood into Bowman’s capsule, forming glomerular filtrate.
Key Features:
- Filtration Membrane: Acts like a coffee filter—allows small molecules (water, glucose, ions) but blocks large ones (proteins, blood cells).
- Filtration Rate (GFR): About 125 mL/min (180 L/day!).
- What’s in the Filtrate?
- Water
- Electrolytes (Na⁺, K⁺, Cl⁻)
- Glucose
- Amino acids
- Waste (urea, creatinine)
Why is This Step Important?
- It’s the first cleanup—removes waste but also keeps useful stuff (which will be reabsorbed later).
- If filtration fails, toxins build up (kidney failure).
Step 2: Tubular Reabsorption – Saving the Good Stuff
The glomerular filtrate is not urine yet it’s just a raw filtrate full of useful substances. The renal tubules now reabsorb what the body needs.
Where Does Reabsorption Happen?
- Proximal Convoluted Tubule (PCT) – The Workhorse
- Reabsorbs 65-70% of filtrate.
- Key Reabsorbed Substances:
- Glucose & Amino acids (via active transport).
- Sodium (Na⁺) (pumps out, water follows).
- Water (via osmosis).
- Fun Fact: Diabetes can overwhelm reabsorption, causing glucose in urine (glycosuria).
- Loop of Henle – The Water & Salt Regulator
- Descending limb: Permeable to water only → water leaves, filtrate concentrates.
- Ascending limb: Permeable to salts only → Na⁺, Cl⁻ pumped out, filtrate dilutes.
- Why This Matters? Creates a salt gradient for water conservation.
- Distal Convoluted Tubule (DCT) – Fine-Tuning
- Adjusts Na⁺, K⁺, Ca²⁺ under hormone control (aldosterone, PTH).
- Example: Aldosterone increases Na⁺ reabsorption (retains water, raises BP).
- Collecting Duct – The Final Water Saver
- Antidiuretic Hormone (ADH) controls water reabsorption.
- No ADH? Dilute urine (like after drinking beer).
- High ADH? Concentrated urine (dehydration).
Why is Reabsorption Critical?
- Prevents loss of essential nutrients.
- Maintains blood volume & pressure.
- Adjusts urine concentration based on hydration.
Step 3: Tubular Secretion – The Cleanup Crew
Not everything unwanted gets filtered out initially. Some toxins, drugs, and excess ions are actively secreted into the tubules.
What Gets Secreted?
- Hydrogen ions (H⁺) – Helps regulate blood pH.
- Potassium (K⁺) – Balances electrolytes.
- Drugs & Toxins (e.g., penicillin, NSAIDs).
Where Does Secretion Happen?
- Mostly in PCT & DCT.
- Example: If blood is too acidic, kidneys secrete more H⁺ to restore balance.
Why is Secretion Important?
- Eliminates substances not initially filtered.
- Fine-tunes pH & electrolyte balance.
The Final Product: Urine Composition
After all three steps, the remaining fluid is urine.
What’s in Urine?
- 95% water
- 5% solutes:
- Urea (from protein breakdown).
- Creatinine (muscle waste).
- Electrolytes (Na⁺, K⁺, Cl⁻).
- Toxins/drugs.
What Shouldn’t Be in Urine?
- Glucose (indicates diabetes).
- Proteins (kidney damage).
- Blood (infection/stones).
Regulation of Urine Formation
The kidneys don’t work alone they’re controlled by:
1. Hormones
- ADH (Vasopressin): Increases water reabsorption → concentrated urine.
- Aldosterone: Increases Na⁺ reabsorption → retains water, raises BP.
- ANP (Atrial Natriuretic Peptide): Opposite of aldosterone → reduces Na⁺ reabsorption → lowers BP.
2. Nervous System
- Sympathetic nerves reduce blood flow to kidneys (e.g., during stress).
3. Blood Pressure & Osmolarity
- Low BP → kidneys conserve water.
- High salt → triggers thirst & ADH release.
Common Disorders Affecting Urine Formation
When this process goes wrong:
- Diabetes Insipidus (ADH deficiency → excessive dilute urine).
- Kidney Stones (crystals form from concentrated urine).
- Acute Kidney Injury (sudden filtration failure).
- Chronic Kidney Disease (gradual loss of function).
Conclusion
Urine formation is a fundamental physiological process carried out by the kidneys to ensure the body’s internal environment remains stable a state known as homeostasis. Through the intricate functions of filtration, reabsorption, secretion, and excretion, the kidneys meticulously regulate the balance of fluids, electrolytes, and waste products.
The kidneys filter approximately 180 liters of blood daily, producing about 1.5 liters of urine. This extensive filtration process allows for the removal of metabolic wastes like urea, creatinine, and excess ions, while conserving essential substances such as glucose, amino acids, and water. By selectively reabsorbing these vital components, the kidneys maintain the body’s electrolyte balance, pH levels, and overall fluid homeostasis.
Moreover, the kidneys play a crucial role in regulating blood pressure through the renin-angiotensin-aldosterone system (RAAS). By adjusting the volume of water and sodium reabsorbed, the kidneys influence blood volume and systemic vascular resistance, thereby contributing to blood pressure regulation.
The process of tubular secretion further enhances the kidneys’ ability to maintain internal balance by eliminating excess hydrogen ions, potassium, and certain drugs. This function is vital for regulating the body’s acid-base balance and preventing the accumulation of potentially harmful substances.
In summary, the physiology of urine formation underscores the kidneys’ indispensable role in sustaining health. Their ability to filter blood, reabsorb essential substances, secrete wastes, and excrete urine ensures that the body operates efficiently and remains in a state of equilibrium. Understanding this complex process highlights the importance of kidney health and the need for practices that support renal function, such as adequate hydration, balanced nutrition, and regular medical check-ups.
Frequently Asked Questions (FAQs)
What is the first step of urine formation?
The first step of urine formation is called glomerular filtration, where your kidneys act like a super-fine sieve. First, your kidneys filter blood like a coffee strainer. Tiny filters catch waste and extra stuff but keep blood cells and proteins. This makes a watery mix ready for cleaning.
What is the process of urine formation?
Urine forms in two key steps: First, kidneys filter blood, removing waste and excess substances. Then, they adjust the filtered fluid reabsorbing useful nutrients and adding extra waste to create urine.
Which condition is favourable for formation of dilute urine?
Dilute urine forms when your body has excess water. This happens with high fluid intake, low blood sodium, or reduced antidiuretic hormone (ADH), which makes kidneys excrete more water while conserving salts. Hot weather or drinking alcohol (which blocks ADH) can also produce pale, watery urine.
Related Articles