What is Oncogenic Virus?
Oncogenic viruses are viruses that can cause cancer in humans and animals. The term “onco” comes from the Greek word for tumor. These viruses can change the way cells grow and divide, often making them multiply uncontrollably. When this happens, tumors can form, which may eventually lead to cancer.
These viruses don’t cause cancer immediately. They often stay in the body for years and only lead to cancer when certain conditions are met. These include a weakened immune system, environmental factors, or other infections.
Summary of Oncogenic virus
- Oncogenic viruses are viruses that can cause cancer by changing the way cells grow and divide.
- Common examples include HPV, EBV, HBV, HCV, HTLV-1, KSHV, and MCV, which can lead to cancers like cervical, liver, and blood cancers.
- These viruses can be prevented or managed through vaccines, safe practices, early detection, and proper medical treatment.
Table of Contents
How Do Viruses Cause Cancer?
Viruses are tiny particles that cannot live or reproduce on their own. They infect living cells and take over their machinery to make more copies of themselves. In some cases, when viruses infect cells, they change the DNA of those cells. These changes can interfere with the normal cell cycle, especially the parts that control cell growth and death.
Normally, our body has “checkpoints” that stop cells from growing out of control. Oncogenic viruses can disrupt these checkpoints by turning off genes that prevent tumors or by turning on genes that help cells grow too fast. Over time, these changes can lead to the formation of cancer.
Types of Oncogenic Viruses in Humans
Several viruses have been identified as oncogenic in humans. These include:
- Human Papillomavirus (HPV)
- Epstein-Barr Virus (EBV)
- Hepatitis B and C Viruses (HBV and HCV)
- Human T-cell Leukemia Virus type 1 (HTLV-1)
- Kaposi’s Sarcoma-associated Herpesvirus (KSHV/HHV-8)
- Merkel Cell Polyomavirus (MCV)
Human Papillomavirus (HPV)
HPV is one of the most well-known cancer-causing viruses. It’s mainly spread through sexual contact. There are over 100 types of HPV, but only a few of them are considered high-risk for cancer.
HPV infects the skin and mucous membranes, and in some people, it causes warts. However, high-risk types like HPV-16 and HPV-18 can cause cancers of the cervix, vagina, penis, anus, and even the throat.
The good news is that there is a vaccine available that protects against the most dangerous types of HPV. This vaccine has already helped reduce HPV infections and cervical cancer cases in many countries.
Epstein-Barr Virus (EBV)
EBV is the virus that causes mononucleosis, also known as “mono” or the “kissing disease.” It is very common and usually infects people during childhood or adolescence.
Although most people recover fully from EBV, the virus can stay in the body for life in a dormant state. In rare cases, EBV is linked to certain cancers like Burkitt lymphoma, Hodgkin lymphoma, and nasopharyngeal carcinoma.
EBV can infect B cells (a type of white blood cell), and in some individuals, it can lead to uncontrolled growth of these cells, causing cancer.
Hepatitis B and C Viruses (HBV and HCV)
HBV and HCV are viruses that mainly affect the liver. They are spread through blood, unprotected sex, and from mother to baby during childbirth. These viruses can cause long-term infections that damage liver cells.
Over time, this damage can lead to chronic liver disease, cirrhosis (scarring of the liver), and liver cancer. The risk is especially high when the infection lasts for many years without proper treatment.
Vaccination against HBV is available and highly effective. For HCV, there is no vaccine yet, but there are excellent treatments that can cure the infection in most cases.
Human T-cell Leukemia Virus Type 1 (HTLV-1)
HTLV-1 is a virus that infects T cells, another type of white blood cell. It is spread through blood, sexual contact, and breastfeeding.
Most people with HTLV-1 don’t develop any symptoms. However, a small number may develop a rare but aggressive cancer called adult T-cell leukemia/lymphoma (ATLL), usually many years after infection.
This virus is more common in certain parts of the world, such as Japan, the Caribbean, and parts of Africa and South America.
Kaposi’s Sarcoma-Associated Herpesvirus (KSHV/HHV-8)
KSHV is linked to a type of cancer called Kaposi’s sarcoma, which forms in the blood vessels of the skin and other organs. This cancer is more common in people with weakened immune systems, such as those with HIV/AIDS.
KSHV can also cause other rare cancers like primary effusion lymphoma and multicentric Castleman disease. It is spread through saliva, and sometimes through sexual contact or blood transfusion.
Kaposi’s sarcoma became widely known during the early years of the AIDS epidemic, when it was seen in many patients with advanced HIV.
Merkel Cell Polyomavirus (MCV)
MCV is a newer discovery. It is associated with Merkel cell carcinoma, a rare but aggressive skin cancer. Most people carry this virus without any problems, but in rare cases, especially in older adults or people with weakened immune systems, it can lead to cancer.
Researchers are still learning more about how MCV causes cancer, but it appears that mutations in the virus may play a key role in the process.
What Increases the Risk of Cancer from These Viruses?
Not everyone who is infected with an oncogenic virus will get cancer. Several factors influence the risk:
- Immune system health: People with weak immune systems, such as those with HIV or those taking immunosuppressant drugs, are more at risk.
- Co-infections: Having more than one infection at the same time can increase the chances of cancer.
- Genetics: Some people may inherit genes that make them more likely to develop cancer when exposed to certain viruses.
- Lifestyle choices: Smoking, alcohol use, poor diet, and unsafe sex can increase the risk of both infection and cancer.
How Can Oncogenic Virus-Related Cancers Be Prevented?
Prevention focuses on stopping infections from happening in the first place or treating them early:
- Vaccination: The HPV and HBV vaccines are safe and effective ways to prevent these infections and reduce cancer risk.
- Safe sex: Using condoms and reducing the number of sexual partners can lower the risk of HPV, HBV, and HIV.
- Screening: Regular medical checkups and screening programs can detect precancerous changes early, especially for cervical and liver cancer.
- Avoiding risky behaviors: Not sharing needles, practicing good hygiene, and avoiding unnecessary blood transfusions can reduce exposure.
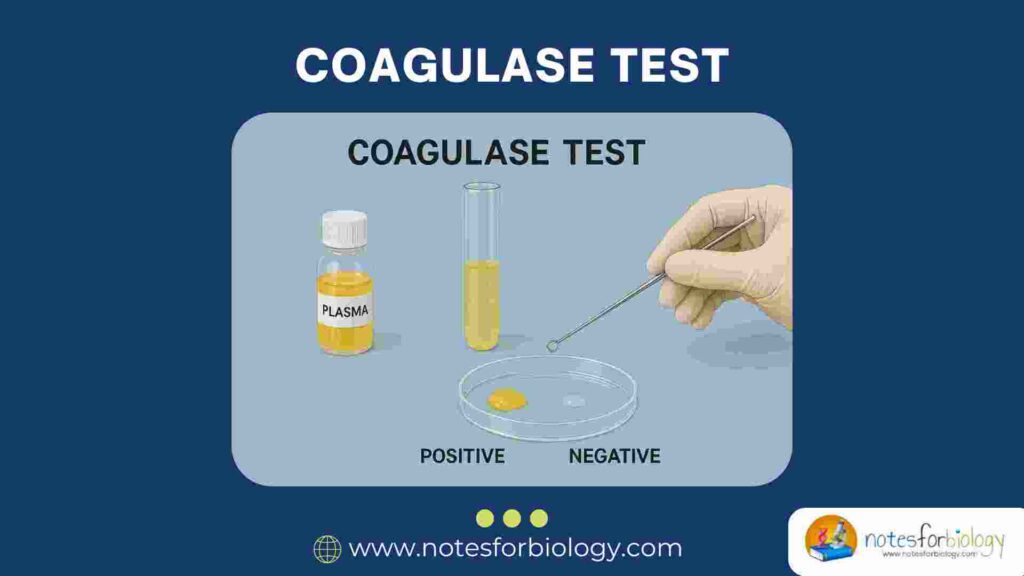
Diagnosing Virus-Linked Cancers
Doctors may use a variety of tests to detect virus-linked cancers. These can include:
- Blood tests: To look for viral infections or markers of cancer.
- Pap smears: To detect changes in the cervix caused by HPV.
- Liver function tests: For people with HBV or HCV.
- Biopsies: Removing a small sample of tissue for examination under a microscope.
Advanced imaging tools like CT scans and MRIs may also be used to find tumors or check if cancer has spread.
Treatment of Virus-Related Cancers
Treatment depends on the type and stage of cancer but can include:
- Surgery: To remove tumors.
- Radiation therapy: To destroy cancer cells.
- Chemotherapy: Drugs that kill fast-growing cells.
- Targeted therapy: Drugs that focus on specific changes in cancer cells.
- Immunotherapy: Boosts the body’s natural defenses to fight cancer.
In some cases, treating the viral infection itself can help prevent or control cancer. For example, antiviral drugs for HBV and HCV can reduce the risk of liver cancer.
Why Research on Oncogenic Viruses Matters
Studying oncogenic viruses helps scientists understand how cancer develops. It also helps in finding new ways to prevent, diagnose, and treat different types of cancer. The discovery of these viruses has already led to the development of life-saving vaccines and treatments.
Ongoing research is also exploring how viruses might be used to fight cancer. For example, scientists are creating modified viruses that can infect and kill cancer cells without harming healthy cells. This approach is called oncolytic virotherapy and holds great promise for the future.
Conclusion
Oncogenic viruses are a significant but often overlooked cause of cancer. While not all infections lead to cancer, understanding the connection helps us take preventive steps and get early treatment. With vaccines, screening, safe practices, and research, we can reduce the number of virus-related cancers and save lives.
Public awareness, access to healthcare, and ongoing scientific discovery all play key roles in this effort. By learning more about oncogenic viruses, we empower ourselves and our communities to take control of our health.
Frequently Asked Questions (FAQs)
Is it common for people with these viral infections to develop cancer?
Not everyone infected with an oncogenic virus will develop cancer. Factors such as immune system strength, genetic predisposition, and environmental exposures play a role in cancer development. However, chronic infections and lack of medical intervention can increase the risk.
What are oncogenic viruses?
Oncogenic viruses are viruses that can cause cancer by altering the normal functions of cells, leading them to grow uncontrollably. These viruses can integrate their genetic material into the host’s DNA, disrupting normal cell regulation.
Which viruses are known to cause cancer in humans?
Several viruses have been linked to human cancers, including:
Human Papillomavirus (HPV): Associated with cervical, anal, and throat cancers.
Hepatitis B and C viruses (HBV and HCV): Linked to liver cancer.
Epstein-Barr Virus (EBV): Connected to certain lymphomas and nasopharyngeal cancer.
Human T-cell Leukemia Virus type 1 (HTLV-1): Causes adult T-cell leukemia/lymphoma.
Kaposi’s Sarcoma-associated Herpesvirus (KSHV/HHV-8): Leads to Kaposi’s sarcoma.
Merkel Cell Polyomavirus (MCV): Associated with Merkel cell carcinoma, a rare skin cancer.
Related Articles