Lymphatic filariasis imposes a significant public health burden, affecting over 120 million people globally, with about 40 million suffering from disabling conditions like lymphedema and elephantiasis. Efforts are ongoing to eliminate the disease through comprehensive control programs aiming to interrupt transmission and alleviate suffering in affected populations.
Table of Contents
Lymphatic filariasis (W. bancrofti)
The parasitic worms Wuchereria bancrofti, Brugia malayi, and Brugia timori are the cause of lymphatic filariasis, which is spread via mosquito bites, mostly from the genera Culex, Anopheles, and Aedes. Tropical and subtropical areas, with their prevalent mosquito breeding grounds and inadequate sanitation, are the primary regions affected by this disease. Efforts are ongoing to eliminate the disease through comprehensive control programs aiming to interrupt transmission and alleviate suffering in affected populations.
Transmission
When a mosquito bites a person who is afflicted, it might carry the larval stage of the microfilariae infection. Within the mosquito, these microfilariae mature into infectious larvae. These larvae are deposited into the skin when an infected mosquito bites a human, where they travel to the lymphatic system and eventually develop into adult worms over a few months.
Pathogenesis
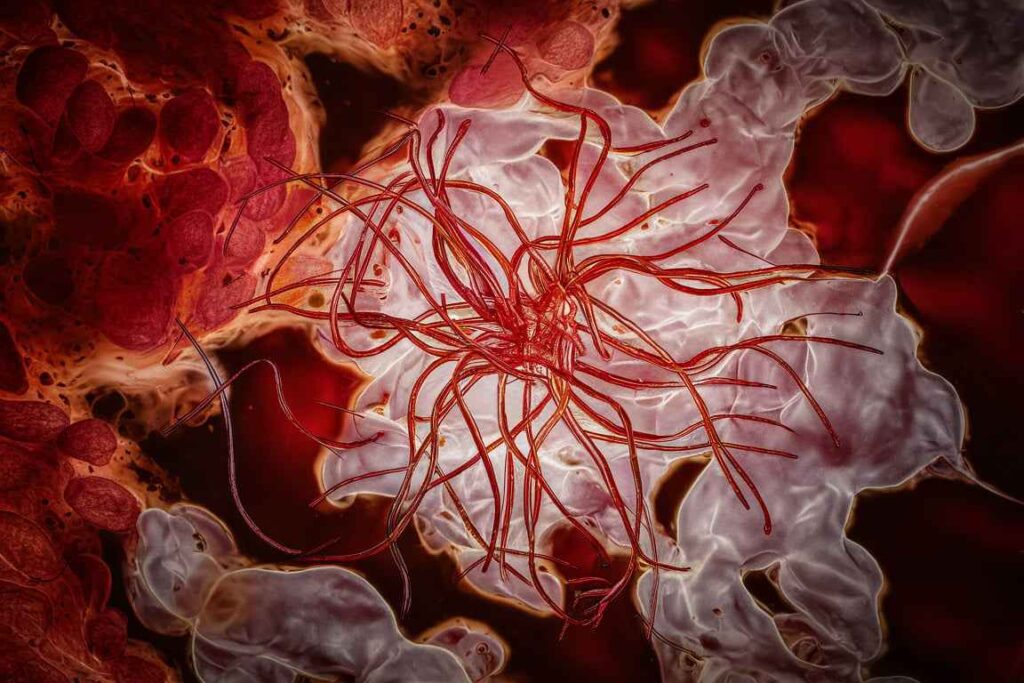
The mature worms go to the lymphatic vessels, where they live and generate microfilariae, marking the start of the infection. The transmission cycle is completed when feeding mosquitoes take up these microfilariae that are circulating in the blood. The prolonged inflammation and blockage caused by adult worms and microfilariae in the lymphatic tubes results in lymphedema, or swelling, lymphatic malfunction, and possibly irreversible harm to the lymphatic tissues.
Adult worms and microfilariae induce tissue damage, immune responses to the parasites, and chronic inflammation and lymphatic dysfunction that result in clinical manifestations such as lymphedema (swelling), elephantiasis (severe swelling of limbs or genitals), and recurrent acute adenolymphangitis (inflammatory episodes).
Clinical Manifestations
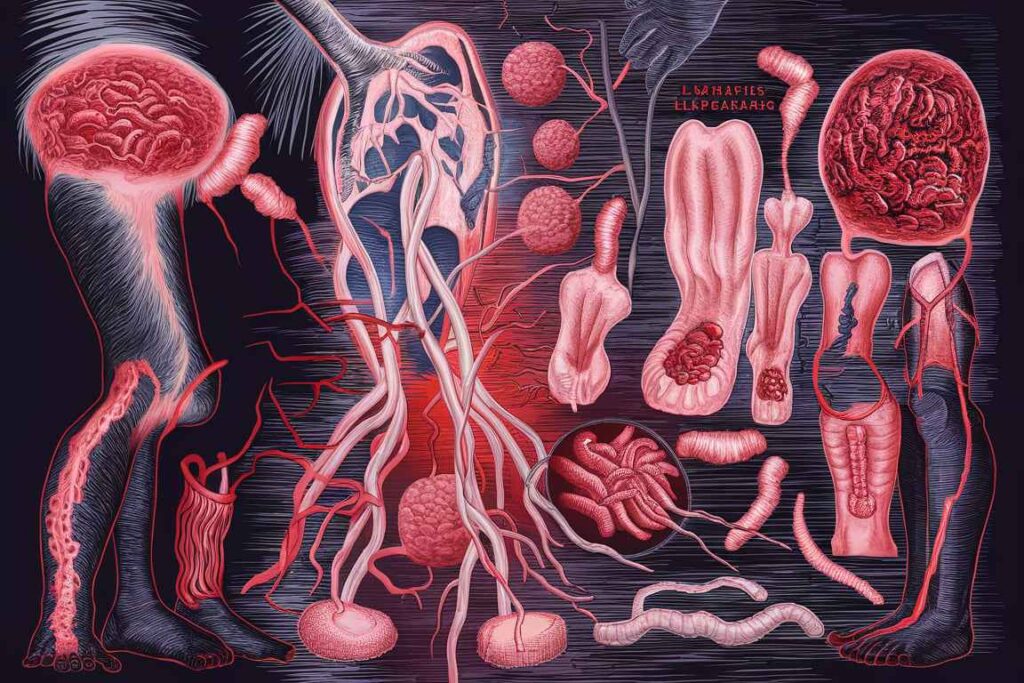
Acute episodes of the disease are characterized by fever, discomfort, and swelling in the affected sites, often the limbs or genitalia. The condition advances slowly. Elephantiasis, which can result in deformity and handicap, and lymphedema, which is characterized by tissue swelling and thickness, are examples of chronic symptoms. Men frequently develop hydrocele, or an accumulation of fluid in the scrotum.
1. Acute Attacks:
Occasional inflammatory episodes (acute adenolymphangitis) characterized by fever, pain, and swelling in the affected limbs or genitals.
2. Chronic Manifestations:
- Lymphedema: Swelling and thickening of the skin in limbs or genitals, often leading to disability and social stigma.
- Elephantiasis: Severe form of lymphedema with tissue fibrosis and thickening, causing grotesque enlargement of limbs or genitals.
- Hydrocele: Accumulation of fluid in the scrotum, common in men.
Diagnosis
Blood samples collected at night, when microfilariae are most likely to be circulating, must be detected in order to make a diagnosis. Antigen detection assays and PCR (Polymerase Chain Reaction) are also used for confirmation.
- Microscopic Analysis: Determination of microfilariae present in blood samples obtained overnight.
- Tests for Identifying Specific Antigens: Identify the antigens that adult worms make.
- Molecular technique used to find parasite DNA in blood samples is called polymerase chain reaction, or PCR.
Treatment
Control measures center on mass drug administration (MDA) to entire at-risk populations of antifilarial drugs like ivermectin or diethylcarbamazine (DEC), frequently in combination with albendazole. These medications stop the spread of microfilariae by killing them. Antibiotics are used in the management of acute episodes, and compression therapy, exercise, and good hygiene are used in the supportive care of patients with lymphedema.
A major global health concern, lymphatic filariasis affects more than 120 million people in tropical and subtropical areas. In an effort to lessen suffering and avoid incapacity brought on by this crippling parasite infection, efforts to eradicate the disease concentrate on vector control, MDA programs, and expanding access to healthcare facilities.
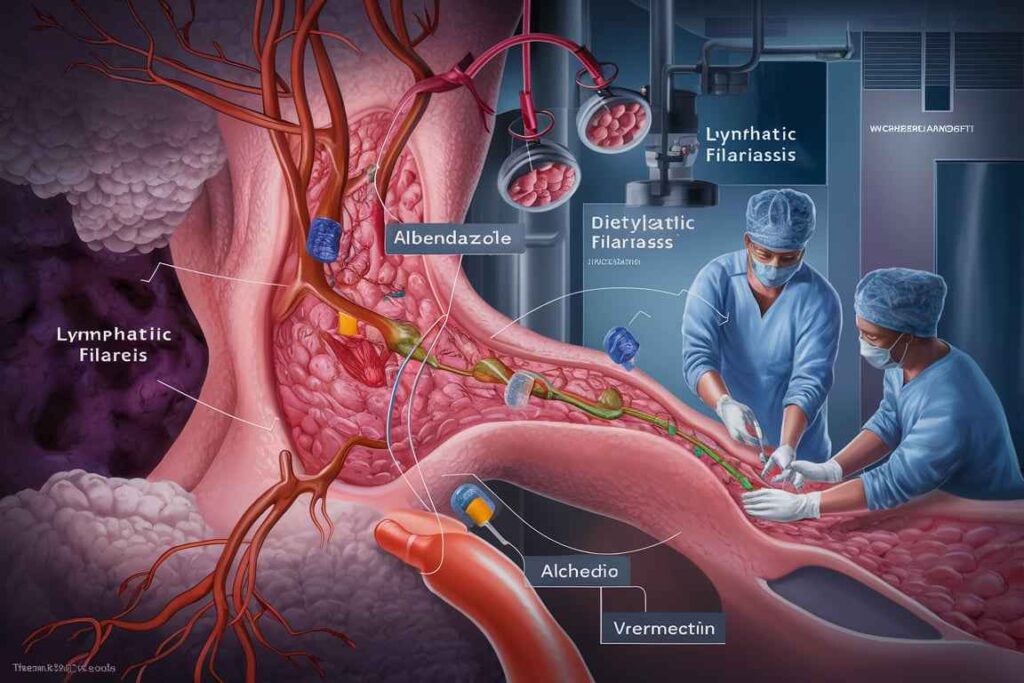
- Mass Drug Administration (MDA): Providing albendazole and antifilarial drugs, such as diethylcarbamazine (DEC) or ivermectin, to all at-risk groups on a yearly or biannual basis.
- Personal Care: Patients who exhibit clinical signs can be treated with antibiotics for acute bouts, and lymphedema can be controlled with proper hygiene, physical activity, and compression therapy.
Public Health Strategies
- Vector Control: Reducing transmission through mosquito control tactics.
- Health education: Encouraging the use of bed nets, protective gear, and good cleanliness.
- Community Engagement: Increasing access to care and treatment services and organizing local communities in support of MDA activities.
Frequently Asked Question
What is Lymphatic filariasis ?
The parasitic worms Wuchereria bancrofti, Brugia malayi, and Brugia timori are the cause of lymphatic filariasis, which is spread via mosquito bites, mostly from the genera Culex, Anopheles, and Aedes.
What is the common name for W bancrofti?
The common name for Wuchereria bancrofti is “filarial worm.”
Which mosquito causes lymphatic filariasis?
The mosquitoes that primarily cause lymphatic filariasis include Culex quinquefasciatus, Anopheles species, and certain Aedes species, depending on the geographic region.
Related Article
Hookworm infection: life cycle, transmission, pathogenesis, diagnosis and treatment