Introduction
Imagine you haven’t eaten for a long time maybe you’re fasting, on a strict diet, or going through intense physical training. Your body needs energy to keep going, especially your brain and red blood cells, which mainly run on glucose (a type of sugar). But what happens when there’s no more sugar left from food?
That’s when your body uses a clever backup system called gluconeogenesis. It’s like your internal sugar factory. The word may sound complicated, but it simply means “making new glucose.”
Table of Contents
What is Gluconeogenesis?
Gluconeogenesis is the natural process by which your body creates glucose (sugar) from non-carbohydrate sources when it doesn’t get enough glucose from food.
It usually kicks in:
- During fasting
- After long periods without eating
- While on a low-carb diet
- During intense exercise
- In certain medical conditions, like diabetes
So, gluconeogenesis helps keep your blood sugar stable, especially when dietary sources of carbohydrates (like rice, bread, fruits) are low.
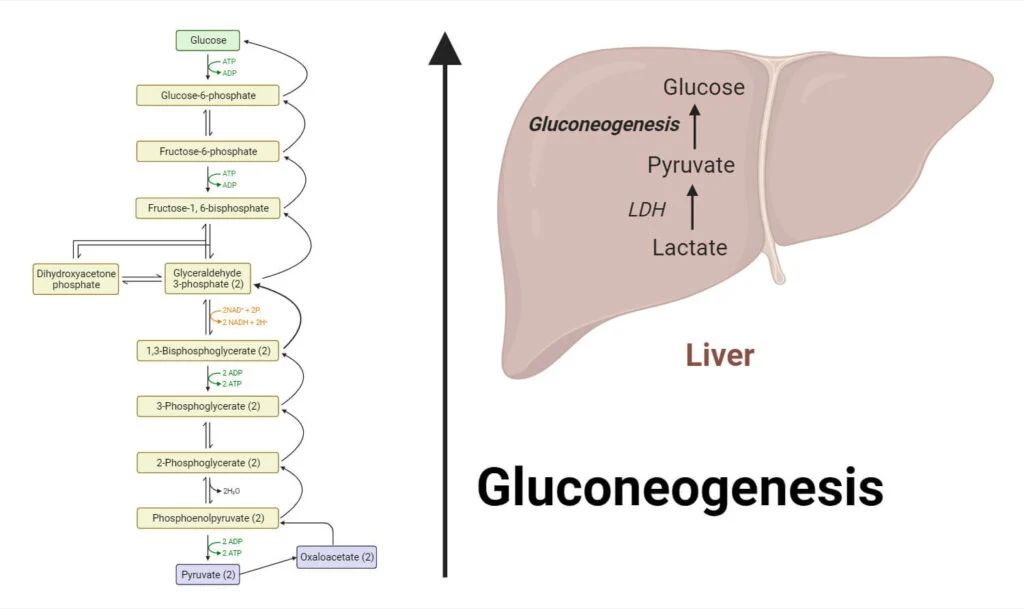
Where Does Gluconeogenesis Happen?
The process mostly happens in the liver and to a lesser extent in the kidneys. These organs have the special enzymes needed to make glucose from other molecules.
Think of the liver as the body’s emergency kitchen—it pulls out ingredients from storage and starts cooking up some glucose when it’s needed most.
Raw Materials for Gluconeogenesis
So, if glucose isn’t coming from food, where does your body get the building blocks to make it?
Here are the main ingredients:
- Lactate
- Produced by muscles during exercise.
- The liver takes it in and turns it back into glucose. (This is part of the Cori cycle.)
- Amino Acids (especially Alanine)
- Come from the breakdown of proteins in your muscles or diet.
- The liver uses them to make glucose when there’s not enough sugar.
- Glycerol
- Comes from fat breakdown.
- When fat is broken down for energy, glycerol is released and can be turned into glucose.
- Pyruvate
- A product of glycolysis (the breakdown of glucose), and a key starting point for many metabolic processes.
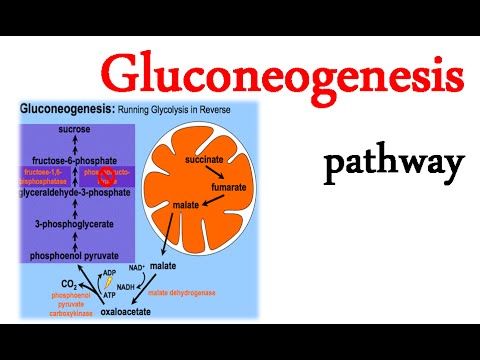
How Does Gluconeogenesis Work?
Gluconeogenesis is not a single step but a pathway made up of many steps, involving several enzymes. It’s like assembling a car in a factory—each step is done by a different machine (enzyme) until the final product (glucose) is ready.
Here’s a simplified overview of the process:
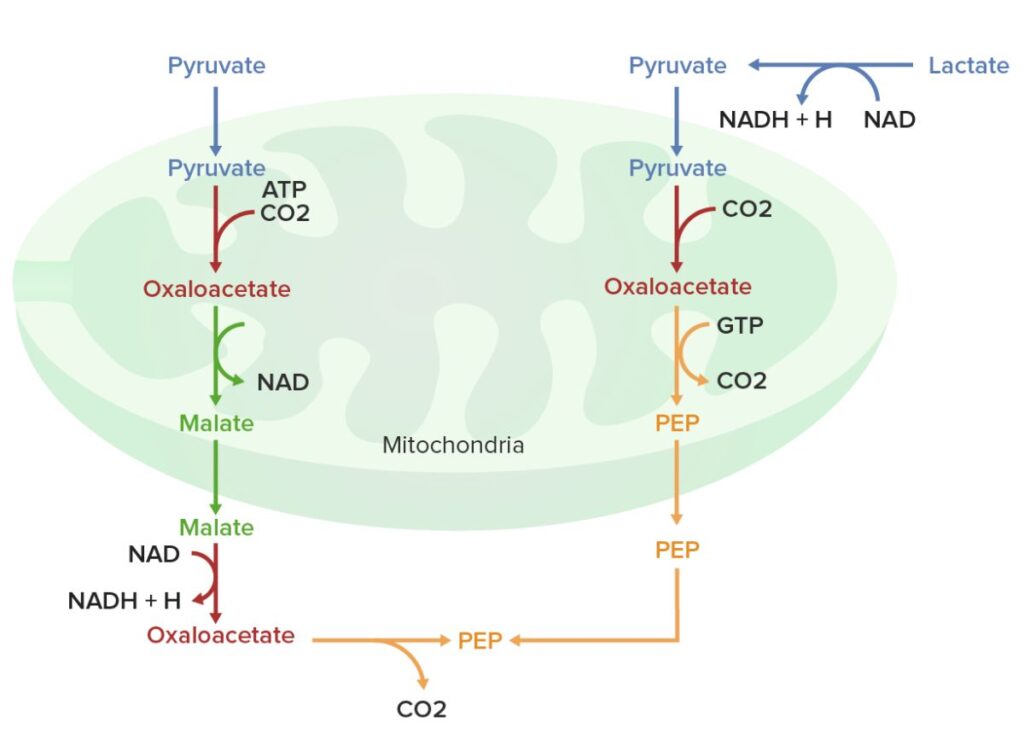
- Starts in the mitochondria with pyruvate (or lactate), which gets turned into oxaloacetate.
- Oxaloacetate is then converted to phosphoenolpyruvate (PEP), a key step requiring a special enzyme.
- Through a series of reactions, PEP is slowly converted into glucose.
- Finally, the newly made glucose is either released into the blood or stored in the liver as glycogen for later use.
Key Enzymes in Gluconeogenesis
There are some important enzymes that control the pace and direction of gluconeogenesis:
- Pyruvate carboxylase
- PEP carboxykinase (PEPCK)
- Fructose-1,6-bisphosphatase
- Glucose-6-phosphatase
These enzymes make sure the process doesn’t go out of control and only happens when the body really needs glucose.
What Regulates Gluconeogenesis?
The body doesn’t allow it to happen all the time. It’s tightly controlled by hormones and energy levels:
Hormones that Control Gluconeogenesis:
- Insulin: Stops gluconeogenesis. When you eat and blood sugar is high, insulin tells the liver to stop making new glucose.
- Glucagon: Stimulates it. When blood sugar drops, glucagon tells the liver to start making glucose.
- Cortisol: A stress hormone that also promotes gluconeogenesis, especially during long-term stress or fasting.
- Epinephrine: In emergencies (like fight or flight), it boosts glucose production for energy.
So, your body is like a smart machine that turns gluconeogenesis on or off depending on the situation.
Why Is Gluconeogenesis Important?
Without gluconeogenesis, your body would run out of glucose very quickly—within hours of your last meal.
Here’s why it’s crucial:
- Keeps the brain running: The brain needs a constant supply of glucose.
- Supports red blood cells: They can’t use fat for energy, only glucose.
- Balances blood sugar levels: Especially between meals or during fasting.
- Protects against low blood sugar (hypoglycemia).
- Helps during starvation or intense exercise.
Gluconeogenesis vs. Glycolysis: What’s the Difference?
These two processes might sound similar, but they’re like opposites:
| Feature | Gluconeogenesis | Glycolysis |
|---|---|---|
| Purpose | Makes glucose | Breaks down glucose |
| Starts from | Non-carbohydrates (like proteins, fats) | Glucose |
| Produces | Glucose | Energy (ATP) |
| Happens during | Fasting, low-carb diet | After eating |
So, gluconeogenesis builds glucose when there isn’t enough, while glycolysis breaks it down when there’s plenty.
Conditions Where Gluconeogenesis Becomes More Active
- Fasting or starvation
- Low-carb or ketogenic diets
- Prolonged exercise or endurance sports
- Uncontrolled diabetes (type 1 or 2)
- Severe stress or trauma
- Hormonal imbalances (high cortisol)
In these situations, it helps keep blood sugar levels from dropping too low.
Clinical Importance of Gluconeogenesis
Understanding this process helps doctors manage conditions like:
1. Diabetes Mellitus
- In type 2 diabetes, it can become overactive, causing high blood sugar levels even if a person isn’t eating much.
- Some diabetes medications work by suppressing it in the liver.
2. Hypoglycemia
- In people who fast too long or have certain metabolic disorders, it may not work properly, leading to dangerously low blood sugar.
3. Starvation
- During long-term starvation, the body relies heavily on gluconeogenesis for survival.
Can Gluconeogenesis Be Harmful?
It’s a life-saving process, but when it’s not properly controlled, it can be harmful:
- In diabetes, too much gluconeogenesis raises blood sugar levels.
- In muscle-wasting conditions, the body breaks down muscle protein to fuel gluconeogenesis, causing weakness.
- In long fasting or starvation, excessive gluconeogenesis can lead to muscle loss and fatigue.
Interesting Facts About Gluconeogenesis
- Your body can produce about 100 grams of glucose per day through gluconeogenesis.
- The brain alone uses about 120 grams of glucose per day!
- Gluconeogenesis uses energy (ATP) — it’s not a free process.
- Newborn babies rely heavily on gluconeogenesis because they can’t store much glycogen.
Conclusion
Gluconeogenesis is one of the most vital processes in your body—it keeps your brain sharp, your red blood cells functioning, and your blood sugar levels steady, especially when food is scarce. It shows just how smart and adaptable your body is. When you’re not eating carbs, your body finds a way to make the sugar it needs by using proteins and fats.
In simple terms, gluconeogenesis is your body’s plan B for survival—a hidden sugar factory that only turns on when it’s truly needed. Understanding this amazing process gives you a deeper appreciation of how your body handles fasting, exercise, and the ups and downs of daily life.
FREQUENTLY ASKED QUESTIONS
What is gluconeogenesis ?
Gluconeogenesis is the process by which your body makes glucose (a type of sugar) from non-carbohydrate sources like proteins, fats, and lactate, especially when you’re not eating enough carbs, such as during fasting, intense exercise, or low-carb diets.
Where does gluconeogenesis occur ?
Gluconeogenesis mainly occurs in the liver and, to a lesser extent, in the kidneys these organs have the special enzymes needed to make glucose from non-carbohydrate sources.
How does insulin inhibit gluconeogenesis ?
Insulin inhibits gluconeogenesis by blocking the activity of key enzymes involved in the process and by reducing the availability of raw materials (like amino acids) needed to make glucose. It also suppresses certain genes that produce gluconeogenesis-related enzymes, effectively signaling the liver to stop making new glucose when blood sugar levels are already high like after eating a meal.
Related Articles