Antibiotic resistance is one of the greatest challenges modern medicine faces, and ESBL -producing bacteria are at the forefront of this problem. Extended Spectrum Beta-Lactamases are enzymes produced by some bacteria that allow them to resist the effects of commonly used antibiotics, specifically penicillins and cephalosporins.
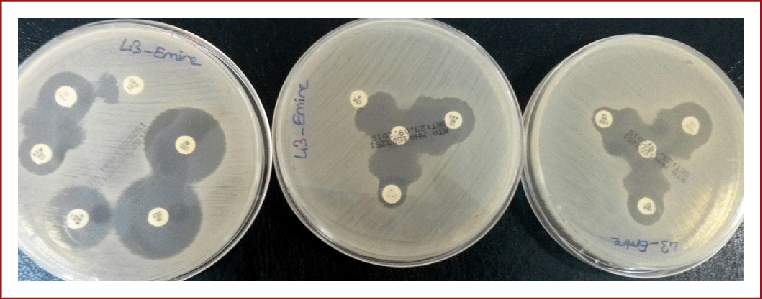
Table of Contents
What are Beta-Lactamases?
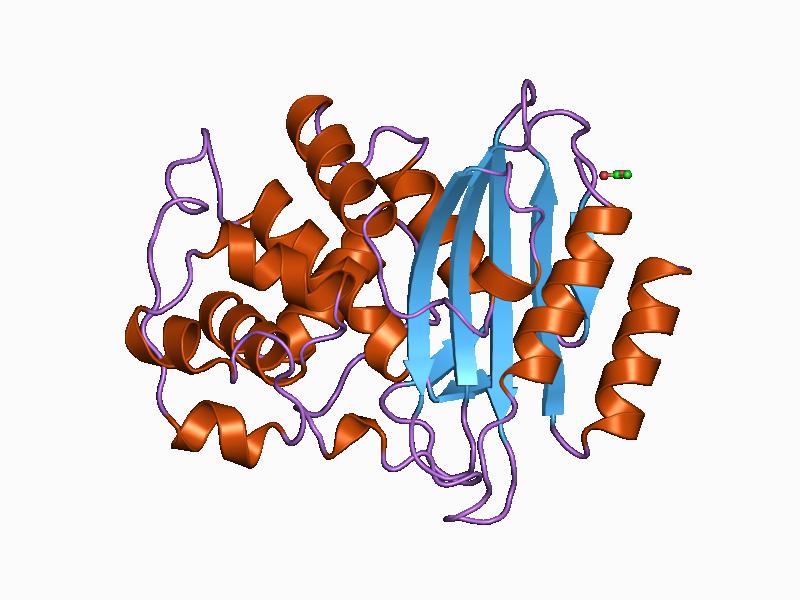
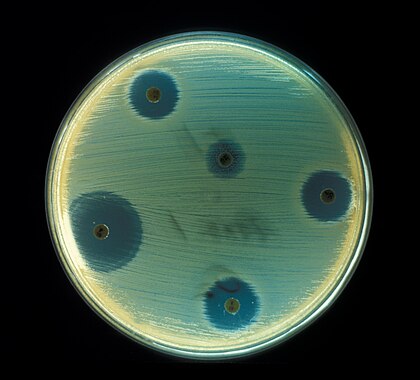
To understand Extended Spectrum beta-Lactamases, let’s start with beta-lactamases. These are enzymes produced by bacteria that break down beta-lactam antibiotics, a group of drugs that includes penicillin, amoxicillin, and cephalosporins. Beta-lactam antibiotics work by targeting the bacterial cell wall, a vital part of the bacteria’s structure. By breaking down these antibiotics, bacteria can survive and continue to grow, despite the presence of the drugs.
ESBLs are a type of beta-lactamase enzyme with a particularly concerning feature: they are capable of breaking down a broader range of antibiotics. These enzymes can deactivate antibiotics like third-generation cephalosporins (such as ceftriaxone and ceftazidime) and monobactams (like aztreonam), which are usually more potent and used for serious infections.
How do ESBLs spread?
Extended Spectrum beta-Lactamases-producing bacteria are most commonly found in the family of bacteria known as Enterobacteriaceae, which includes common culprits like Escherichia coli (E. coli) and Klebsiella pneumoniae. These bacteria are normal inhabitants of the human gut but can become harmful if they develop Extended Spectrum beta-Lactamases and cause infections such as urinary tract infections (UTIs), pneumonia, bloodstream infections, and even more severe conditions.
The spread of Extended Spectrum beta-Lactamases-producing bacteria is primarily driven by the overuse or misuse of antibiotics. The more often bacteria are exposed to antibiotics, the greater the chance that resistant strains will emerge. Poor hygiene in hospitals, clinics, and nursing homes can also contribute to the spread of Extended Spectrum beta-Lactamases bacteria, as they can move from one person to another through contaminated surfaces or medical equipment.
Types of ESBLs
There are several different types of Extended Spectrum beta-Lactamases enzymes, each with its own characteristics and ability to break down antibiotics. Here are a few of the most common types:
TEM-type ESBLs
The TEM enzyme was one of the first beta-lactamases discovered in the 1960s. It was named after the patient from whom it was isolated (Temoniera). Mutations in the TEM enzyme have led to the development of Extended Spectrum beta-Lactamases, allowing these bacteria to resist a wide range of beta-lactam antibiotics. TEM-1 and TEM-2 are the most common, but there are now more than 200 variants of the TEM enzyme.
SHV-type ESBLs
SHV stands for “sulfhydryl variable.” SHV enzymes are closely related to TEM and are often found in Klebsiella pneumoniae. Like TEM enzymes, SHV enzymes can undergo mutations that enhance their ability to break down third-generation cephalosporins. SHV-1 is the most basic form, but SHV-2 and SHV-5 are examples of variants that display Extended Spectrum beta-Lactamases activity.
CTX-M-type ESBLs
The CTX-M family of Extended Spectrum beta-Lactamases is named for its potent ability to hydrolyze cefotaxime, a third-generation cephalosporin. CTX-M enzymes have become one of the most common Extended Spectrum beta-Lactamases types worldwide and are often found in E. coli. They pose a significant public health challenge due to their widespread dissemination and high resistance to beta-lactam antibiotics. CTX-M-15 is one of the most frequently encountered subtypes globally.
OXA-type ESBLs
OXA stands for oxacillin-hydrolyzing, and this group of enzymes has a slightly different structure compared to TEM, SHV, and CTX-M types. OXA enzymes are often associated with Acinetobacter species and can also be found in Pseudomonas aeruginosa. OXA-type enzymes are concerning because they can resist a broad range of beta-lactam antibiotics and often go undetected in standard screening tests.
Implications for Treatment
When a bacterial infection involves Extended Spectrum beta-Lactamases-producing bacteria, treating it becomes much more difficult. Many of the commonly used antibiotics are ineffective, and doctors must turn to more specialized and often more expensive or toxic options. Carbapenems, for example, are usually effective against ESBL-producing bacteria, but the overuse of these drugs is now leading to carbapenem resistance as well.
In addition to carbapenems, other treatment options include:
Beta-lactamase inhibitors: These are drugs like clavulanic acid and tazobactam that can inhibit the action of ESBL enzymes. They are often used in combination with beta-lactam antibiotics to help restore their effectiveness.
Non-beta-lactam antibiotics: Some infections may require the use of antibiotics from other classes, such as aminoglycosides, quinolones, or polymyxins, although resistance to these drugs is also on the rise.
Prevention and Control
To control the spread of Extended Spectrum beta-Lactamases-producing bacteria, a combination of strategies is necessary:
Judicious use of antibiotics: Avoiding unnecessary antibiotic prescriptions is key to reducing the chances of resistance. Only using antibiotics when they are truly needed and ensuring the full course is completed helps minimize the chances of bacteria developing resistance.
Infection control in healthcare settings: Hospitals and clinics must implement strict hygiene and infection control practices, such as handwashing, using gloves and gowns, and sterilizing equipment. This helps prevent the spread of resistant bacteria between patients.
Surveillance: Monitoring the emergence and spread of Extended Spectrum beta-Lactamases producing bacteria in both healthcare and community settings can help identify outbreaks and guide treatment decisions.
Conclusion
ESBL-producing bacteria represent a growing challenge in healthcare worldwide. By understanding the types of Extended Spectrum beta-Lactamases, how they spread, and the strategies available for treatment and prevention, we can take important steps to slow down the rise of antibiotic resistance and protect public health.
Frequently Asked Questions(FAQ)
Define CTX-M-type ESBLs?
The CTX-M family of Extended Spectrum beta-Lactamases is named for its potent ability to hydrolyze cefotaxime, a third-generation cephalosporin. CTX-M enzymes have become one of the most common Extended Spectrum beta-Lactamases types worldwide and are often found in E. coli.
Define antibiotics?
Drugs known as antibiotics treat bacterial illnesses in both humans and animals. They function by either eradicating the germs or hindering their ability to proliferate. Antibiotics can be administered in various ways: verbally (via the mouth).
Related Articles