Introduction
Enterotoxigenic E. coli (ETEC) is one of the most common causes of diarrhea, especially in young children living in developing countries and in travelers visiting these regions. This type of bacteria is known for producing special toxins that affect the intestines, leading to watery diarrhea that can become severe if not properly managed. ETEC is a specific group of E. coli bacteria that can make people sick when they consume contaminated food or water. Unlike some other harmful bacteria that directly damage the cells of the intestines, ETEC causes illness mainly by producing toxins that disturb the normal function of the intestines.
Learning about ETEC is very important for healthcare providers, scientists, travelers, and people working in public health. This guide provides a detailed yet simple explanation of what ETEC is, how it works, the symptoms it causes, how it is diagnosed and treated, and how people can protect themselves from getting infected.
Table of Contents
What Is Enterotoxigenic E. coli (ETEC)?
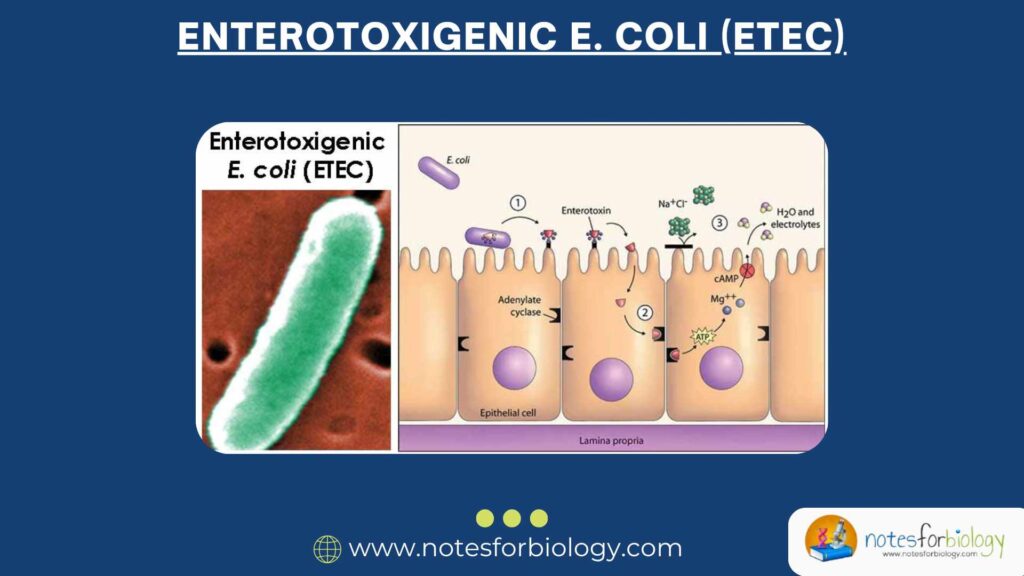
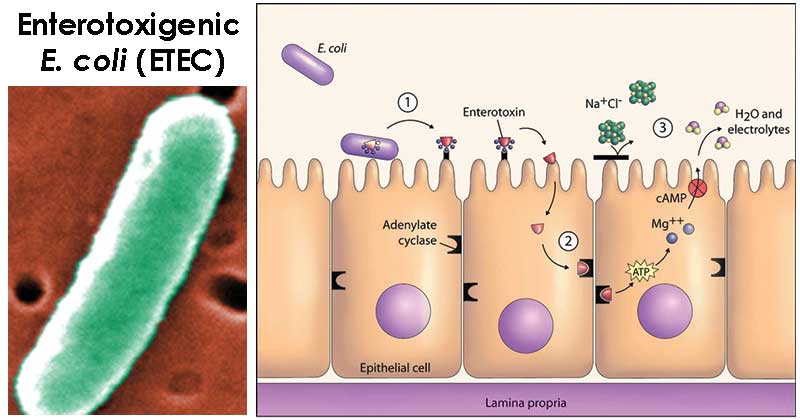
ETEC is a specific kind of Escherichia coli, a bacterium that normally lives in the intestines of humans and animals. Most E. coli strains are harmless and even helpful, but some strains, like ETEC, can cause disease. Enterotoxigenic E. coli (ETEC) produces toxins that affect the intestines, causing diarrhea. It does not invade the intestinal walls but instead stays on the surface and releases harmful substances known as enterotoxins. These toxins interfere with the body’s natural ability to absorb water and electrolytes, which leads to the rapid loss of fluids.
Because it doesn’t break into the cells of the intestines, Enterotoxigenic E. coli (ETEC) is called a “non-invasive” pathogen. However, it still causes serious symptoms by creating a toxic environment in the gut, making it difficult for the body to function normally.
Structure and Features of Enterotoxigenic E. coli (ETEC)
ETEC shares many physical features with other E. coli bacteria. It is a Gram-negative, rod-shaped bacterium. Some of the important parts that help it survive and cause disease include:
- Fimbriae (Pili): These are tiny hair-like structures on the surface of the bacteria. They help Enterotoxigenic E. coli (ETEC) stick tightly to the walls of the intestine. Without fimbriae, the bacteria would be flushed out of the gut.
- Flagella: These are whip-like tails that help the bacteria move. They allow Enterotoxigenic E. coli (ETEC) to travel through the watery environment of the intestines to reach suitable areas for colonization.
- Outer membrane: The outer covering of the bacteria contains molecules like lipopolysaccharides (LPS), which play a role in protecting the bacteria and triggering the immune response in humans. This membrane also helps the bacteria resist harsh environments.
These structural parts make ETEC better equipped to survive in the intestines and cause illness.
How Enterotoxigenic E. coli (ETEC) Causes Disease (Pathogenesis)
Enterotoxigenic E. coli (ETEC) causes illness by producing two main types of toxins that interfere with normal digestion and absorption of fluids:
1. Heat-labile toxin (LT)
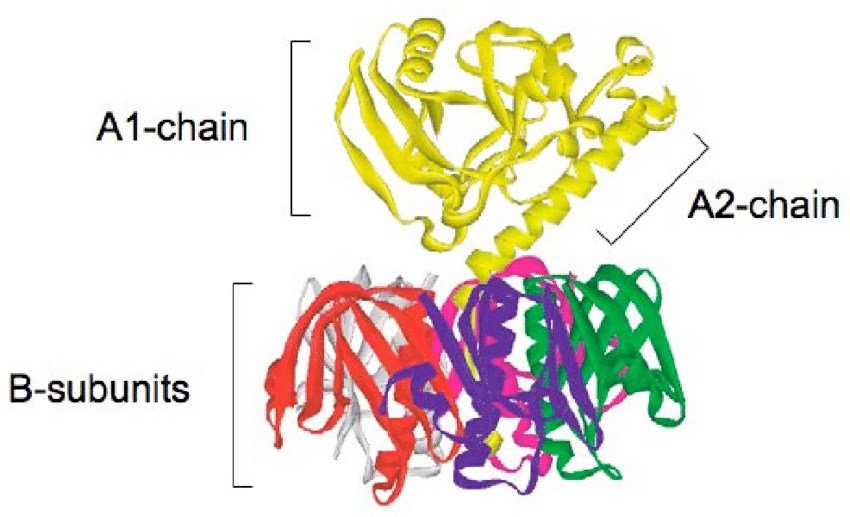
- This toxin is sensitive to heat, meaning it can be destroyed at high temperatures.
- Its structure is similar to the toxin produced by Vibrio cholerae, the bacterium that causes cholera.
- It affects intestinal cells by increasing a substance called cyclic AMP (cAMP), which tells the cells to release chloride ions into the gut.
- As chloride is released, water follows, leading to watery diarrhea.
2. Heat-stable toxin (ST)
- Unlike LT, this toxin is not destroyed by heat.
- It increases another chemical inside the cells called cyclic GMP (cGMP).
- Just like LT, this leads to the release of water and electrolytes from the intestinal cells into the lumen of the gut.
ETEC bacteria usually produce either one or both of these toxins. Once they reach the intestines, they use fimbriae to stick to the walls and then release the toxins, starting the process that leads to diarrhea.
Transmission
ETEC is spread primarily through the fecal-oral route. This means a person can get infected if they consume food or water that has been contaminated with feces from an infected person. Poor sanitation, unclean drinking water, and improper food handling all contribute to the spread of ETEC.
Some common ways the bacteria can spread include:
- Eating raw or undercooked food, especially meat or seafood.
- Drinking water from unsafe sources, such as untreated tap water, lakes, or rivers.
- Eating fruits and vegetables that were not properly washed.
- Touching contaminated surfaces or hands and then putting them in the mouth.
- Food prepared by individuals who did not wash their hands after using the toilet.
Who Is at Risk?
Anyone can get sick from ETEC, but some people are more vulnerable than others. These include:
- Infants and young children: Their immune systems are not fully developed, and they are more likely to suffer from dehydration.
- Travelers to developing countries: People from developed nations often lack immunity to local strains of ETEC and are commonly affected by Traveler’s Diarrhea.
- People with weakened immune systems: Individuals with chronic diseases or those undergoing treatments that weaken the immune system are at higher risk of severe illness.
Symptoms
ETEC symptoms typically appear within 1 to 3 days after a person is exposed to the bacteria. The illness usually lasts between 3 to 7 days, though it can be shorter or longer depending on the person’s overall health.
Common symptoms include:
- Watery diarrhea: The diarrhea is usually not bloody and can be quite severe, leading to significant fluid loss.
- Abdominal cramps: Pain or discomfort in the stomach area due to irritation in the intestines.
- Nausea: A feeling of wanting to vomit, sometimes accompanied by actual vomiting.
- Fever: A mild increase in body temperature as the immune system responds to the infection.
- Fatigue: A person may feel tired or weak due to dehydration and the loss of nutrients.
In most healthy individuals, these symptoms resolve on their own. However, if not treated properly, they can lead to dehydration, especially in children or elderly people.
Diagnosis
Diagnosing ETEC can be challenging because its symptoms are similar to many other causes of diarrhea. In most cases, especially in resource-limited settings, doctors make a diagnosis based on symptoms and the person’s travel or exposure history.
When available, laboratory tests can help:
- Stool culture: Growing the bacteria from a stool sample. However, this does not always identify ETEC specifically.
- PCR (Polymerase Chain Reaction): This advanced test detects the specific genes responsible for producing LT and ST toxins.
- ELISA (Enzyme-Linked Immunosorbent Assay): A test that identifies ETEC toxins in the stool sample.
- Rapid diagnostic kits: These are being developed to quickly detect ETEC in field conditions, especially useful in outbreak investigations.
Treatment
Treatment of ETEC infection focuses on replacing the fluids and electrolytes lost during diarrhea. In most cases, the body will recover with simple supportive care.
Rehydration
- Oral Rehydration Salts (ORS): These are packets containing a mix of salt and sugar that help the body absorb water more efficiently. They are mixed with clean water and sipped frequently.
- Intravenous (IV) fluids: In cases of severe dehydration or if the person cannot drink, fluids are given directly into the veins.
Antibiotics
Antibiotics are not always needed but may be given if the symptoms are moderate to severe. They can help reduce the duration of diarrhea and bacterial shedding:
- Ciprofloxacin: A commonly used antibiotic for bacterial diarrhea.
- Azithromycin: Useful for resistant strains and also safe for children and pregnant women.
- Rifaximin: A non-absorbed antibiotic that acts locally in the gut, suitable for travelers’ diarrhea.
Zinc Supplementation
Zinc is especially helpful in children with diarrhea. It strengthens the immune system and helps the intestines recover faster.
Prevention
Preventing ETEC infection is possible with good hygiene and safe food practices.
Personal Hygiene
- Wash hands thoroughly with soap and clean water before eating or preparing food.
- Always wash hands after using the toilet or handling diapers.
- Use hand sanitizers when soap is not available.
Food Safety
- Drink only water that has been boiled, filtered, or bottled from a trusted source.
- Avoid ice in drinks unless you are sure it was made from clean water.
- Eat only well-cooked food served hot.
- Wash or peel fruits and vegetables before eating.
Traveler’s Tips
- Use bottled water even for brushing teeth.
- Carry ORS packets and zinc tablets in your travel kit.
- Avoid street food unless it is freshly cooked and served hot.
Vaccine Development
As of now, there is no widely available vaccine specifically for ETEC. However, researchers are working on vaccines that target ETEC toxins and fimbriae.
Some oral cholera vaccines like Dukoral offer partial protection against ETEC, especially for short-term travelers. The goal is to develop a vaccine that is effective, affordable, and covers the many different types of ETEC found around the world.
Enterotoxigenic E. coli (ETEC) vs Other E. coli Pathotypes
It’s helpful to know how ETEC differs from other harmful strains of E. coli:
| Pathotype | Key Features |
|---|---|
| ETEC | Produces enterotoxins LT and/or ST |
| EHEC (STEC) | Produces Shiga toxin, may cause bloody stool |
| EPEC | Damages intestinal lining, mostly in infants |
| EAEC | Forms biofilm, causes persistent diarrhea |
| EIEC | Invades intestinal cells, similar to Shigella |
| DAEC | Diffusely adherent, less clearly defined role |
ETEC is different because it does not damage cells directly or cause bloody diarrhea. It mainly causes watery diarrhea through toxins.
Complications
Most ETEC infections are mild and resolve with basic care. But in some people, complications can occur:
- Severe dehydration: Loss of too much water and salts can lead to dizziness, weakness, and in severe cases, even death.
- Electrolyte imbalance: Important salts like sodium and potassium are lost in diarrhea, leading to muscle cramps, confusion, or irregular heartbeat.
- Malnutrition: In children, frequent infections can interfere with growth and absorption of nutrients.
- Secondary infections: A weakened gut may become vulnerable to other bacteria or viruses.
Public Health Importance
Enterotoxigenic E. coli (ETEC) is a leading cause of illness and death from diarrhea in children under five years of age in many low-income countries. It is also responsible for millions of lost school days, workdays, and healthcare costs. Controlling ETEC is an important step in improving public health, especially for vulnerable populations.
Ongoing Research on Enterotoxigenic E. coli (ETEC)
Scientists are actively working to better understand and control ETEC infections:
- Developing vaccines that provide broad protection.
- Creating rapid tests that can be used in clinics or during outbreaks.
- Exploring new treatments that work without contributing to antibiotic resistance.
- Studying how ETEC spreads in communities to improve public health strategies.
Conclusion
Enterotoxigenic E. coli (ETEC) is a serious cause of diarrhea, especially in children and travelers. It works by producing toxins that cause fluid to be released into the intestines, leading to watery diarrhea. Although often self-limiting, ETEC can lead to dangerous dehydration and other complications in certain individuals.
Preventing Enterotoxigenic E. coli (ETEC) through better sanitation, hygiene, and safe food and water practices is currently the best approach. Ongoing research promises hope for future vaccines and better treatments. With proper knowledge and precautions, the burden of ETEC-related illness can be significantly reduced.
Three Key Summary of Enterotoxigenic E. coli (ETEC)
- Enterotoxigenic E. coli (ETEC) causes diarrhea by releasing toxins that disturb the intestinal fluid balance, leading to watery stool.
- Infections spread through contaminated food or water and are common in developing countries and among travelers.
- Good hygiene, safe eating practices, and future vaccines are key to prevention.
Frequently Asked Questions
How do I know if I have ETEC?
If you experience watery diarrhea within a few days of traveling to a new area or after eating food of questionable cleanliness, ETEC could be the cause. Only lab tests can confirm it.
Can ETEC cause bloody diarrhea?
No, ETEC usually causes watery, non-bloody diarrhea. If blood is present, another type of infection like EHEC might be involved.
Can I catch ETEC from someone else?
Direct person-to-person spread is not common, but poor hand hygiene can increase the risk, especially in shared living conditions.
Related Articles