What is Coxiella burnetii ?
Coxiella burnetii is the bacterium that causes Q fever, a disease that can be transmitted from animals to humans. This small, Gram-negative bacterium can withstand tough environmental conditions, making it highly resilient. Let’s dive into its habitat, how it spreads, the process of infection, the diseases it causes, diagnostic methods, and treatment options.
Table of Contents
Habitat
Coxiella burnetii primarily lives in farm animals like sheep, goats, and cattle, which are considered its natural reservoirs. These animals often carry the bacteria without showing signs of illness. It is most concentrated in animal products such as the placenta, urine, feces, and milk, particularly during birthing, when large amounts of the bacterium are released.
What sets C. burnetii apart is its ability to survive outside of its host for long periods. It can persist in soil, dust, and other environmental surfaces for months or years, waiting to be inhaled by a new host. In its spore-like form, it resists extreme environmental conditions, including heat and dryness.
Transmission
Humans most often contract Coxiella burnetii by inhaling contaminated dust or particles from animal products like wool, manure, or birth fluids. Q fever outbreaks are typically associated with areas where livestock is raised, such as farms. Less frequently, humans can get infected by direct contact with animals or by consuming unpasteurized dairy products.
After entering the human body through inhalation, the bacteria settle in the lungs and can spread to other parts of the body through the bloodstream, leading to infection. Human-to-human transmission is very rare.
Pathogenesis (Disease Development)
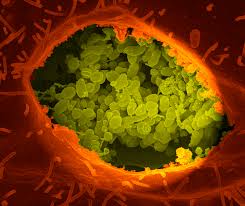
Once inside the body, Coxiella burnetii infects macrophages, which are immune cells that usually fight off infections. The bacteria replicate within these cells, leading to an immune response. Despite the body’s efforts to eliminate it, C. burnetii can remain in the body for long periods, causing persistent infections.
There are two forms of Q fever: acute and chronic. Acute Q fever develops soon after infection, while chronic Q fever can take months or even years to develop, particularly in individuals with weakened immune systems or heart conditions.
Symptoms and Clinical Diseases
Acute Q Fever
Acute Q fever usually manifests 2 to 3 weeks after exposure, with symptoms resembling the flu, such as:
- High feverSevere headacheMuscle painFatigueChillsCough (which can lead to pneumonia)
Chronic Q fever
Chronic Q fever is less common but much more severe. It primarily affects individuals with underlying conditions, such as heart valve issues or compromised immune systems. Chronic Q fever often leads to endocarditis (infection of the heart valves), which can be life-threatening without treatment. It may also affect bones or blood vessels.
Laboratory Diagnosis
Since the symptoms of Q fever can resemble other illnesses, laboratory tests are essential for a definitive diagnosis. Common methods include:
Serology: This blood test detects antibodies the body produces to fight Coxiella burnetii, which helps confirm an infection.

PCR (Polymerase Chain Reaction): This method identifies the bacteria’s genetic material in blood or tissue samples, providing a more direct diagnosis.

Culture: Growing the bacteria in a lab is possible but difficult because of its specific growth requirements, so it’s not commonly used for routine diagnosis.
Treatment
Acute Q fever is treated with antibiotics, with doxycycline being the most commonly prescribed. Treatment is most effective when started early and usually lasts about two weeks. Most people recover fully with timely antibiotic therapy.
Chronic Q fever, particularly cases involving endocarditis, requires long-term antibiotic treatment, often a combination of doxycycline and hydroxychloroquine, which may need to be continued for months or even years to completely eliminate the bacteria and prevent recurrence.
In severe cases, such as when heart valves or other organs are significantly damaged by the chronic infection, surgery may be required.
Conclusion
Coxiella burnetii, the bacteria that causes Q fever, thrives in livestock and is capable of surviving in the environment for extended periods. It spreads to humans through contaminated dust or animal products. While many cases of Q fever cause mild symptoms, the infection can become severe, especially in chronic cases. Early detection and prompt antibiotic treatment are critical for recovery, and preventive measures in farming communities are key to controlling outbreaks.
Frequently Asked Questions (FAQ)
Describe the transmission of Coxiella burnetii ?
Humans most often contract Coxiella burnetii by inhaling contaminated dust or particles from animal products like wool, manure, or birth fluids. Q fever outbreaks are typically associated with areas where livestock is raised, such as farms. Less frequently, humans can get infected by direct contact with animals or by consuming unpasteurized dairy products.
What are the two forms of Q fever?
The two forms of Q fever are Acute Q fever and chronic Q fever.
Related Articles