Introduction
Corynebacterium diphtheriae, commonly known as the Klebs-Löffler bacillus, is a Gram-positive bacterium that causes diphtheria, a serious and potentially life-threatening infection. Discovered by Edwin Klebs and Friedrich Löffler in the late 19th century, this bacterium became infamous for its role in respiratory and cutaneous infections before the advent of effective vaccination.

Though diphtheria is now rare in developed countries due to widespread immunization, it remains a threat in regions with low vaccine coverage. This document presents a comprehensive and simplified understanding of Corynebacterium diphtheriae — its structure, classification, pathogenesis, clinical features, diagnosis, treatment, prevention, and global impact.
Table of Contents
General Characteristics of Corynebacterium diphtheriae
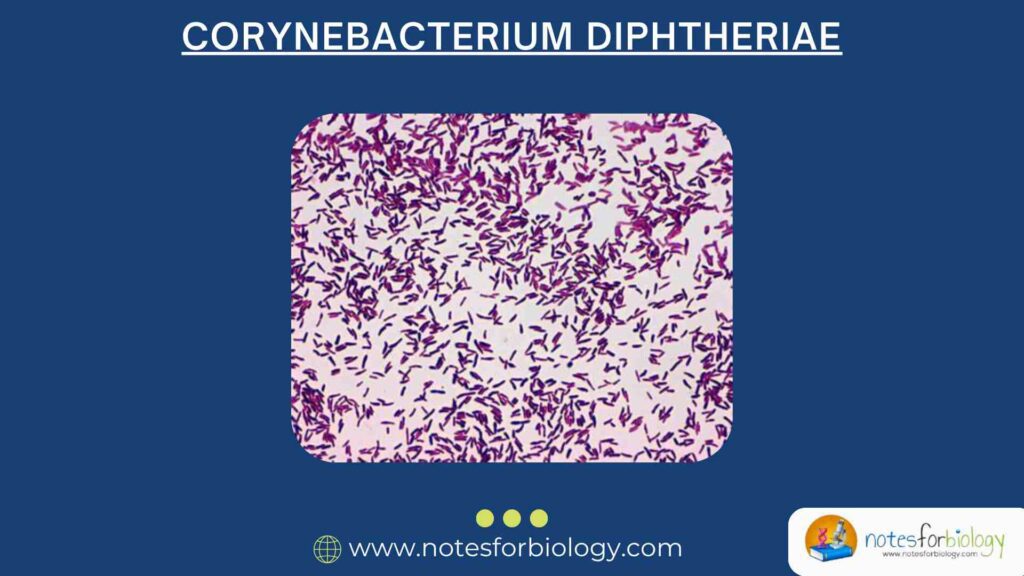
Morphology
- Shape: Rod-shaped (bacillus)
- Gram reaction: Gram-positive
- Arrangement: Characteristic “Chinese letter” or V-shaped arrangements
- Spore formation: Non-spore forming
- Motility: Non-motile
- Size: Approximately 1–8 µm in length
- Staining: Exhibits metachromatic granules (Babes-Ernst granules) when stained with Albert’s stain
Growth Characteristics
- Aerobic or facultative anaerobic
- Optimum temperature: 37°C
- Culture media:
- Löffler’s serum slope (for rapid growth and granule visualization)
- Potassium tellurite agar (selective medium)
- Blood agar (for hemolysis observation)
Classification and Biotypes
Corynebacterium diphtheriae is classified into four biotypes based on colony morphology and biochemical reactions:
1. Gravis
- Large, gray-black colonies
- Rough and raised
- Associated with severe disease
2. Mitis
- Smaller, smooth colonies
- Generally causes milder infections
3. Intermedius
Characteristics between Gravis and Mitis
4. Belfanti
Rare biotype, usually non-toxigenic
Habitat and Transmission of Corynebacterium diphtheriae
Natural Habitat
- Human nasopharynx and skin
- Only known reservoir: Humans
Mode of Transmission
- Droplet infection: From coughing, sneezing, or speaking
- Direct contact: With cutaneous lesions or contaminated surfaces
- Fomites: Rare but possible via contaminated objects
Toxin Production and Pathogenesis
Diphtheria Toxin
The primary cause of disease is a potent exotoxin produced by toxigenic strains. Only strains infected by a lysogenic beta-phage produce the toxin.
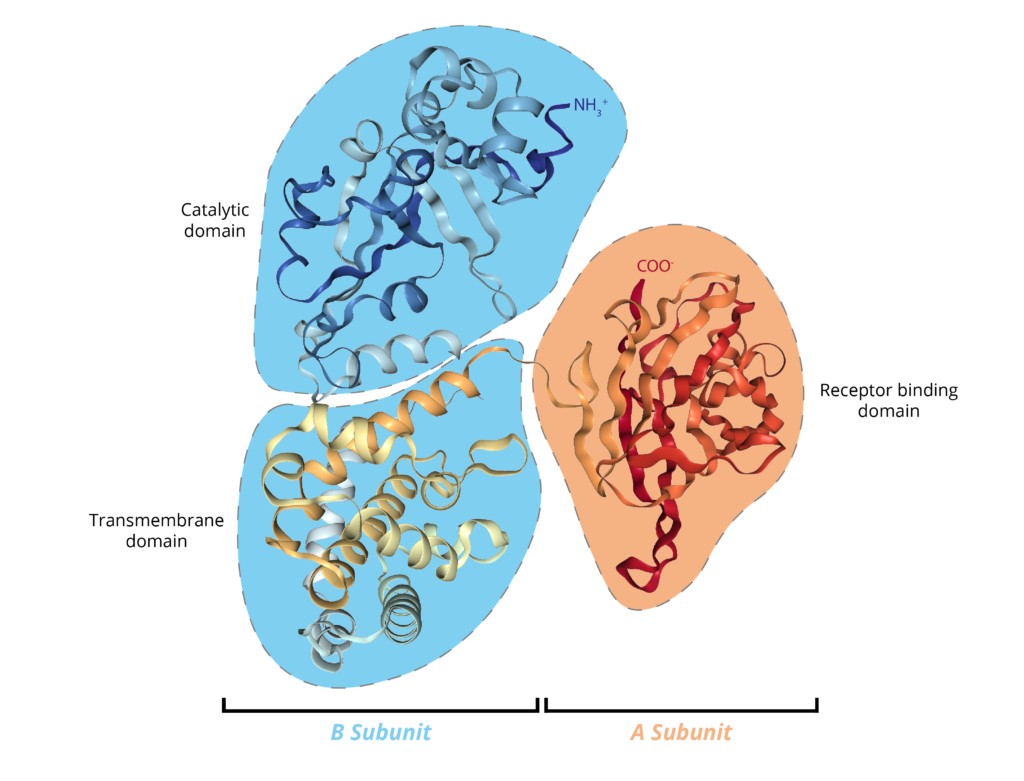
Structure of the Toxin:
- A-B exotoxin:
- A subunit: Active part that inhibits protein synthesis
- B subunit: Binds to host cell receptors
Mechanism of Action:
- Toxin binds to host cell via B subunit
- Enters the cell through endocytosis
- A subunit inactivates elongation factor-2 (EF-2)
- Protein synthesis stops → cell death
Effects on the Body:
- Local necrosis and inflammation
- Formation of a grayish pseudomembrane in the throat
- Systemic toxin spread can affect heart (myocarditis), nerves (neuritis), and kidneys
Clinical Manifestations
1. Respiratory Diphtheria
- Sore throat, low-grade fever, and malaise
- Pseudomembrane formation: Gray, adherent layer on tonsils, pharynx, or larynx
- Swelling of neck lymph nodes → “Bull neck” appearance
- Difficulty breathing; stridor
- Can progress to airway obstruction
2. Cutaneous Diphtheria
- Chronic, non-healing skin ulcers
- Common in tropical regions and among homeless populations
3. Systemic Complications
- Myocarditis: Arrhythmia, heart failure
- Neuropathy: Paralysis, especially of soft palate
- Renal failure (in rare cases)
Laboratory Diagnosis
Specimen Collection
- Throat swabs: From pseudomembrane and throat
- Skin swabs: From cutaneous lesions
Microscopy
- Albert’s stain: Shows green bacilli with bluish-black granules
- Gram stain: Shows Gram-positive rods
Culture
- Löffler’s medium: Enhances granule formation
- Potassium tellurite agar: Black or gray colonies due to tellurite reduction
Toxin Detection
- Elek’s gel precipitation test: Detects diphtheria toxin production
- PCR and ELISA: For toxin gene detection
Treatment of Diphtheria
1. Antitoxin Therapy
- Neutralizes circulating diphtheria toxin
- Must be given early, before toxin binds to cells
- Derived from horse serum → requires sensitivity testing
2. Antibiotics
- Help eliminate the bacteria and stop further toxin production
- Common choices:
- Erythromycin (oral or IV)
- Penicillin G
3. Supportive Care
- Oxygen therapy if airway is blocked
- IV fluids, cardiac monitoring, and mechanical ventilation if needed
4. Isolation
To prevent spread, patients should be isolated until cultures are negative
Prevention and Control
1. Vaccination
- DTP (Diphtheria, Tetanus, Pertussis) vaccine is the main preventive measure
- Given in multiple doses during childhood
- Booster doses recommended every 10 years
2. Public Health Measures
- Prompt identification and treatment of cases
- Screening and treatment of close contacts
- Ensuring high vaccination coverage in the community
3. Prophylaxis for Contacts
Antibiotics (e.g., erythromycin) and booster vaccination
Epidemiology and Global Scenario
Historical Impact
- Major cause of child mortality before vaccines
- Severe epidemics in early 20th century
Current Situation
- Rare in developed countries due to vaccines
- Still endemic in parts of Asia, Africa, and Latin America
- Outbreaks occur in areas with low immunization or conflict zones
Corynebacterium diphtheriae in the Laboratory
Identification Tests
- Catalase test: Positive
- Urease test: Negative
- Nitrate reduction: Positive
- Sugar fermentation patterns help differentiate biotypes
Differentiation from Non-Toxigenic Corynebacteria (Diphtheroids)
- Normal flora may look similar under the microscope
- Only toxigenic strains cause disease
- Requires toxin testing (Elek test or PCR)
Challenges in Diphtheria Management
1. Vaccine Hesitancy
- Misinformation and lack of access
- Decrease in herd immunity
2. Delayed Diagnosis
Lack of awareness in non-endemic areas
3. Drug Resistance
Rare, but surveillance is necessary
4. Resource Limitations
In low-income settings, lack of access to antitoxins and diagnostics
Conclusion
Corynebacterium diphtheriae is a classic example of how a small bacterium can cause a life-threatening illness, especially if left untreated. The diphtheria toxin, not the bacteria itself, is the main villain, damaging tissues far from the infection site. Thanks to vaccination, diphtheria has become a rare disease in many parts of the world, but it remains a global health threat where immunization programs are weak or disrupted.
Early diagnosis, administration of antitoxin, appropriate antibiotics, and high vaccination coverage are the cornerstones of prevention and management. Healthcare providers must stay vigilant, especially during outbreaks or in populations with poor immunization.
FREQUENTLY ASKED QUESTIONS
What causes diphtheria?
The bacterium Corynebacterium diphtheriae, especially its toxin-producing strains.
How is diphtheria transmitted?
Mainly through respiratory droplets or direct contact with infected lesions.
What is the role of the diphtheria toxin?
It stops protein synthesis in cells, leading to cell death and systemic complications.
Related Articles