Introduction
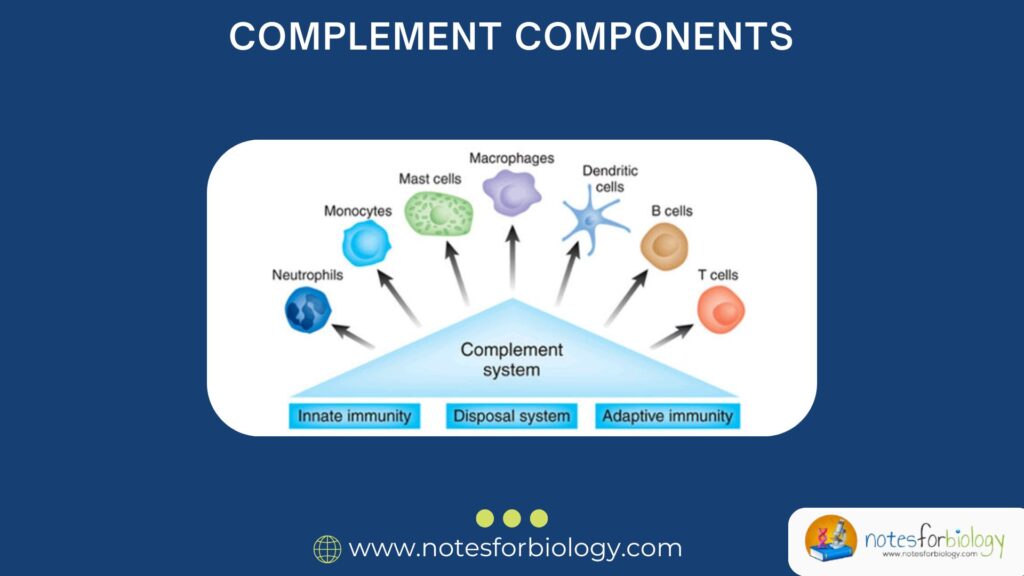
Complement components are a group of specialized proteins found in the blood and on cell surfaces that make up the complement system, which is a vital part of our immune defense. These components are usually labeled C1 to C9, along with some additional proteins like Factor B, Factor D, Properdin, MBL (mannose-binding lectin), and regulatory proteins like Factor H, I, DAF, CD59, etc.
Key Points:
- Most complement components are produced by the liver.
- They circulate in the blood in an inactive form.
- When the immune system detects a threat like a bacterium, virus, or fungus, these components are activated in a precise sequence (called a cascade).
- They help destroy pathogens, alert other immune cells, and clean up the site of infection.
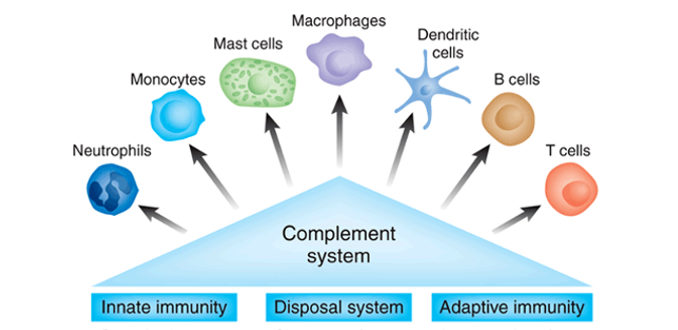
The immune system is a complex and highly organized defense mechanism that protects our body from harmful invaders such as bacteria, viruses, and fungi. One of the most powerful tools in this system is the complement system. Though the name might sound like a supporting actor in a movie, the complement system plays a lead role in immunity. It acts like a rapid-response team, attacking invaders, helping other immune cells recognize threats, and cleaning up the mess after an infection.
This article will explain what complement components are, how they work, and the 7 major functional categories they fall into — all in a simple, clear, and human-friendly way.
Table of Contents
What is the Complement System?
Definition:
The complement system is a part of the immune system made up of over 30 proteins found in the blood plasma and on cell surfaces. These proteins work together in a cascade-like manner to fight infections.
Origin:
Most complement proteins are produced in the liver and are normally found in an inactive state. When triggered by the presence of a pathogen (like bacteria), these proteins become active and start a chain reaction that leads to:
- Killing of the pathogen directly
- Attracting immune cells to the site of infection
- Enhancing the ability of immune cells to do their job
Basic Terminology
- Complement Components: These are the individual proteins, usually labeled C1 to C9.
- Activation Pathways: There are three main ways the complement system can be activated:
- Classical Pathway (triggered by antibodies)
- Alternative Pathway (triggered by pathogen surfaces)
- Lectin Pathway (triggered by sugars on microbes)
Complement Components – Overview
The key complement components are:
1. C1 Complex
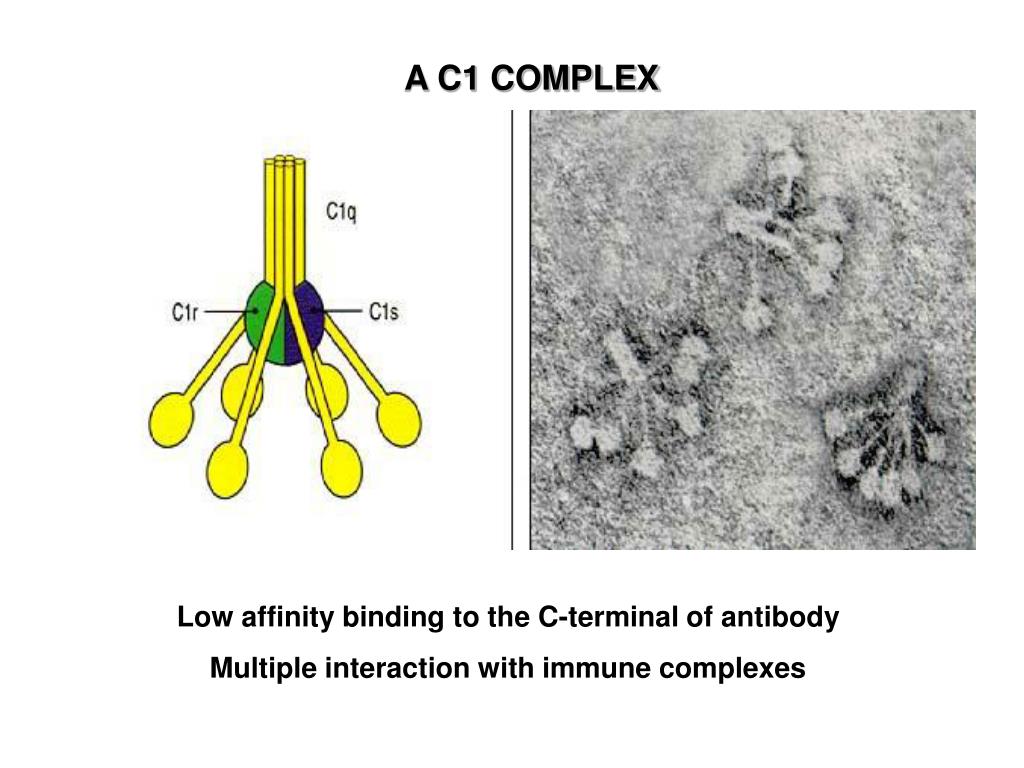
- Made of three parts: C1q, C1r, and C1s
- Initiates the classical pathway when antibodies are bound to antigens
2. C2 and C4
- Work with the C1 complex to form C3 convertase, an important enzyme in the cascade
3. C3
- The central and most important protein in all pathways
- When activated, C3 splits into C3a and C3b
- C3b attaches to pathogens, making them easier to identify and destroy
4. C5 to C9
- These form the membrane attack complex (MAC)
- MAC creates holes in the pathogen’s membrane, leading to cell death
The 7 Functional Categories of Complement components System
Complement proteins don’t all do the same thing. They are divided into 7 main functional categories, each with a unique role in immunity:
1. Initiators
These are the proteins that recognize a danger signal (like a virus or bacterium) and start the complement cascade.
Key Players:
- C1q (Classical Pathway) – binds to antibodies
- MBL (Mannose-Binding Lectin) – binds to sugars on microbes (Lectin Pathway)
Function:
- Detect invaders
- Trigger the first steps in the complement cascade
2. Enzymes (Convertases)
These enzymes break down complement components to activate them.
Key Players:
- C3 convertase – breaks down C3 into C3a and C3b
- C5 convertase – breaks down C5 into C5a and C5b
Function:
- Amplify the immune response
- Activate other components to continue the cascade
3. Opsonins
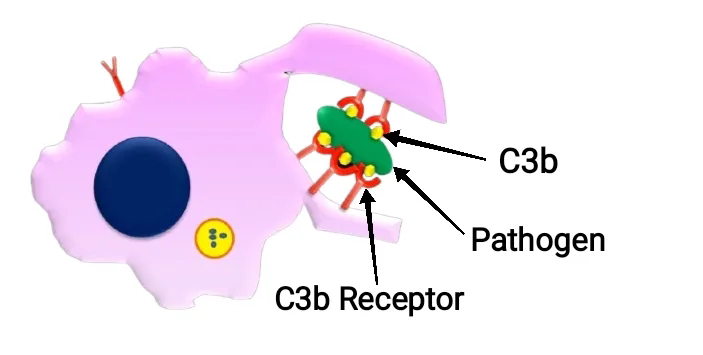
Opsonins “tag” pathogens so that immune cells can recognize and eat them more easily.
Key Players:
- C3b – binds to the surface of pathogens
- C4b – works similarly but less powerful than C3b
Function:
Mark invaders for destruction (like putting a “kick me” sign on them for immune cells)
4. Anaphylatoxins (Inflammatory Mediators)
These small fragments promote inflammation, alerting the body to infection.
Key Players:
C3a, C4a, C5a
Function:
- Attract immune cells to the site of infection (chemotaxis)
- Increase blood vessel permeability
- Trigger release of histamine and other inflammatory chemicals
5. Membrane Attack Complex (MAC) Components
These proteins come together to punch holes in the membranes of invading cells.
Key Players:
C5b, C6, C7, C8, C9
Function:
- Form a pore in the membrane of the pathogen
- Cause water to rush in, bursting the cell (lysis)
6. Regulatory Proteins
These proteins make sure the complement system doesn’t harm our own cells.
Key Players:
- Factor H, Factor I – stop unnecessary activation
- DAF (Decay Accelerating Factor) – breaks down convertases on our cells
- CD59 – blocks MAC formation on human cells
Function:
- Protect host cells
- Maintain balance and prevent autoimmunity
7. Complement Receptors
These are found on immune cells and help them detect complement-tagged invaders.
Key Players:
- CR1 (Complement Receptor 1) – binds C3b
- CR2, CR3, CR4 – bind other fragments
Function:
- Allow immune cells to recognize and bind to pathogens coated in complement
- Help activate B cells (CR2)
- Enhance phagocytosis and clearance
How the Complement components System Works Step-by-Step
Let’s walk through a basic sequence:
- Recognition: C1q or MBL binds to the pathogen.
- Activation: Enzyme convertases are formed.
- Amplification: C3 is split; more components are activated.
- Opsonization: C3b coats the microbe.
- Inflammation: C3a and C5a summon white blood cells.
- Lysis: C5b initiates MAC; pathogen is destroyed.
- Regulation: Host cells are protected by regulatory proteins.
Importance of Complement components in Health and Disease
Protective Roles:
- Defends against bacterial, viral, and fungal infections
- Works with antibodies for stronger immune attacks
- Clears dead cells and immune complexes
Medical Relevance:
- Complement deficiencies can lead to repeated infections
- Overactivation can cause diseases like lupus, kidney damage, or even contribute to COVID-19 complications
- New treatments called complement inhibitors (like eculizumab) are used in rare diseases
Real-Life Examples
Example 1: Bacterial Infections
In bacterial meningitis, the complement system is activated. C3b tags the bacteria, and MAC helps destroy it.
Example 2: Autoimmune Disorders
In lupus, the complement system may attack the body’s own tissues due to poor regulation.
Example 3: Hereditary Angioedema
A rare disease caused by a deficiency in a regulatory protein (C1 inhibitor), leading to uncontrolled swelling.
Conclusion
The complement system is like a team of secret agents within your body — always ready to recognize threats, call in backup, tag enemies, destroy them, and make sure innocent bystanders aren’t harmed. It is composed of a network of proteins working in harmony across seven functional categories: initiators, enzymes, opsonins, anaphylatoxins, MAC components, regulatory proteins, and complement receptors. Each plays a unique role in protecting us from disease and maintaining balance in our immune system.
Understanding this elegant system not only helps us appreciate our body’s natural defense but also guides scientists in developing therapies for infections, autoimmune conditions, and inflammation-related diseases.
FREQUENTLY ASKED QUESTIONS
Is the complement system part of innate or adaptive immunity?
It is mainly a part of the innate immune system, but it also supports the adaptive system by working with antibodies.
What happens if complement components are missing?
Deficiencies can lead to frequent infections, autoimmune diseases, or inflammatory disorders.
Can the complement system be harmful?
Yes, if not properly regulated, it can attack the body’s own cells and contribute to diseases like lupus or kidney inflammation.
Related Articles