In clinical microbiology laboratories, accurate detection and identification of pathogenic bacteria are critical for diagnosis and treatment. Enriched media play an essential role in cultivating fastidious organisms that cannot grow on simple nutrient media.
One of the most widely used enriched media is Columbia Agar with 5% Sheep Blood. This medium is valued for its ability to support the growth of a broad range of bacteria while enabling the observation of hemolytic reactions, which are diagnostically significant in identifying pathogens.
Table of Contents
Importance of Enriched Media in Clinical Microbiology
Enriched media contain additional nutrients, growth factors, or blood components that support the growth of fastidious microorganisms. In medical microbiology, these media help recover pathogens from clinical specimens like blood, sputum, and throat swabs, ensuring no potential infectious agent is missed.
Columbia Agar with 5% Sheep Blood is particularly important for its enhanced nutrient profile and its ability to differentiate bacteria based on hemolytic patterns — a crucial diagnostic feature in infections caused by Streptococci and other organisms.
Brief Overview of Columbia Agar with 5% Sheep Blood
Columbia Agar with 5% Sheep Blood is a general-purpose, non-selective enriched medium widely used for isolating and cultivating fastidious and non-fastidious bacteria. Its composition allows excellent recovery of pathogens and offers clear visualization of hemolysis types surrounding bacterial colonies.
This medium is particularly valued in clinical bacteriology for throat, wound, sputum, and blood cultures where hemolysis provides clues to the pathogen’s identity.
What is Columbia Agar with 5% Sheep Blood?
This section explains the definition, classification, and origin of Columbia Agar, along with its unique role among blood-containing culture media.
Definition and Classification
Columbia Agar with 5% Sheep Blood is a nutrient-rich, enriched medium consisting of Columbia Agar Base supplemented with sterile defibrinated sheep blood. It is classified as an enriched, differential medium because it enhances the growth of fastidious organisms and differentiates bacteria based on hemolysis patterns.
This medium belongs to the broader category of blood agars, yet its specific formulation with Columbia base provides superior nutritive capacity compared to conventional blood agar bases.
Historical Background of Columbia Agar
It was first developed at Columbia University in the 1940s as a highly nutritious medium for clinical bacteriology. Its formulation was designed to support a broad range of pathogenic bacteria, including Streptococcus species, which require enriched conditions.
The addition of 5% sheep blood further expanded its utility by enabling the observation of hemolysis, making it a staple in diagnostic laboratories worldwide.
Composition of Columbia Agar with 5% Sheep Blood
The effectiveness of this medium lies in its carefully balanced composition, which provides nutrients for bacterial growth and facilitates hemolysis detection.
List of Main Ingredients
The primary components of Columbia Agar with 5% Sheep Blood include:
- Peptones (Pancreatic digest of casein and peptic digest of animal tissue)
- Corn starch
- Sodium chloride
- Agar
- Defibrinated sheep blood (5%)
- Distilled water
Each of these components serves a specific function in ensuring optimal bacterial growth and facilitating differential hemolysis.
Role of Each Component
Peptones
Peptones are enzymatic digests of proteins that provide essential amino acids, nitrogen, vitamins, and growth factors required by a wide variety of organisms, including fastidious species like Streptococci.
Corn Starch

Corn starch acts as a neutralizing agent, absorbing potential toxic metabolites produced during bacterial growth. It also stabilizes the medium, supporting the growth of hemolytic streptococci and enhancing hemolysin production.
Sodium Chloride
Sodium chloride maintains osmotic balance within the medium, ensuring bacterial cells remain intact and capable of normal metabolic activities throughout the incubation period.
Agar
Agar serves as the solidifying agent, forming a stable medium surface for colony development. Its inert nature ensures it doesn’t interfere with microbial metabolism or hemolysis reactions.
Sheep Blood (5%)
Defibrinated sheep blood provides additional nutrients such as hemin and growth factors and acts as a differential agent. It allows the observation of hemolytic patterns around bacterial colonies, crucial for differentiating pathogenic species, especially Streptococcus.
Nutrient Contributions to Microbial Growth
Together, these ingredients create a highly supportive environment, making Columbia Agar superior to simpler nutrient agar formulations. The enriched base coupled with blood supplements allows the recovery of both non-fastidious and demanding fastidious organisms while also enabling the study of hemolysis types.
Principle of Columbia Agar with 5% Sheep Blood
This section highlights how the medium works to support bacterial growth and differentiate species based on their ability to lyse red blood cells.
How It Supports Bacterial Growth
The Columbia Agar base supplies essential nutrients, while 5% sheep blood enhances the growth of fastidious organisms and provides an opportunity to observe hemolytic reactions. Blood components like hemin and NAD (nicotinamide adenine dinucleotide) are essential for certain pathogens.
Bacteria inoculated onto the medium metabolize the available nutrients, proliferate, and either utilize or lyse red blood cells depending on their enzymatic capabilities.
Hemolysis Reaction Interpretation

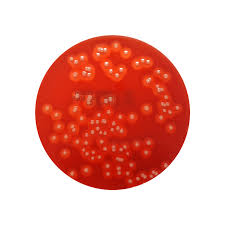
Bacterial colonies growing on blood-containing media may produce hemolysins that lyse red blood cells, resulting in distinct hemolysis patterns observable around colonies.
Alpha Hemolysis
Alpha hemolysis is characterized by a partial, greenish discoloration of the medium around colonies, caused by the oxidation of hemoglobin to methemoglobin. This reaction is typical of Streptococcus pneumoniae and some viridans group streptococci.
Beta Hemolysis
Beta hemolysis involves complete lysis of red blood cells and hemoglobin, producing a clear, colorless zone surrounding the colonies. It is exhibited by pathogens like Streptococcus pyogenes and Staphylococcus aureus.
Gamma Hemolysis
Gamma hemolysis, or non-hemolysis, refers to the absence of red blood cell lysis around bacterial colonies. The medium remains unchanged, typically seen with organisms like Enterococcus faecalis.
Preparation of Columbia Agar with 5% Sheep Blood
Correct preparation is essential for maintaining the medium’s nutritional integrity and hemolytic properties.
Materials and Reagents Required
- Columbia Agar Base powder
- Defibrinated sheep blood (sterile, 5%)
- Distilled water
- Autoclave
- Sterile Petri dishes
Step-by-Step Preparation Process
- Suspend the prescribed amount of Columbia Agar Base powder in distilled water.
- Heat to boiling to dissolve completely.
- Autoclave at 121°C for 15 minutes.
- Cool the medium to 45–50°C.
- Aseptically add 5% sterile, defibrinated sheep blood.
- Mix gently to avoid bubble formation.
- Pour into sterile Petri dishes and allow to solidify.
Precautions During Preparation
Avoid overheating or adding blood to excessively hot medium, as this may denature blood proteins and alter hemolysis reactions. Blood must be added aseptically to prevent contamination, and thorough mixing without frothing is essential for uniform distribution.
Quality Control of Columbia Agar
Ensuring medium performance is crucial for reliable diagnostic results. Quality control involves testing known organisms and inspecting for sterility, correct hemolysis patterns, and medium clarity.
Performance Testing
Standard strains exhibiting known hemolytic behaviors are inoculated onto prepared plates. The medium should support expected growth rates and reproduce characteristic hemolysis patterns.
Recommended Control Organisms
- Streptococcus pyogenes (Beta hemolysis)
- Streptococcus pneumoniae (Alpha hemolysis)
- Enterococcus faecalis (Gamma hemolysis)
Expected Results and Interpretation
Accurate interpretation of colony morphology and hemolysis patterns provides crucial diagnostic information.
Colony Morphology on Columbia Agar
Different bacteria form distinctive colonies in terms of size, shape, elevation, and pigmentation. Streptococci typically produce small, translucent colonies, while Staphylococci may appear larger and opaque.
Hemolysis Patterns and Their Diagnostic Significance
The type of hemolysis observed helps differentiate closely related bacterial species, particularly within the Streptococcus genus. For instance, distinguishing Streptococcus pyogenes (beta hemolytic) from Streptococcus pneumoniae (alpha hemolytic) is vital for appropriate clinical management.
Uses of Columbia Agar with 5% Sheep Blood
Columbia Agar with 5% Sheep Blood remains one of the most versatile and widely utilized enriched media in clinical, research, and pharmaceutical microbiology. Its broad-spectrum utility comes from its enriched nutritional content and ability to reveal hemolytic reactions.
This section elaborates on its primary applications in healthcare, diagnostic labs, and research settings.
Routine Clinical Microbiology Applications
In diagnostic laboratories, Columbia Agar with 5% Sheep Blood is routinely employed for primary isolation of bacterial pathogens from clinical specimens such as throat swabs, sputum, wound exudates, and blood cultures. Its enriched formulation ensures fastidious and non-fastidious bacteria alike can be recovered efficiently.
Particularly, it is indispensable for diagnosing respiratory infections, sepsis, and skin and soft tissue infections, especially those involving streptococcal and staphylococcal species.
Detection of Fastidious Organisms
Fastidious bacteria like Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus species require additional nutrients for growth, which Columbia Agar provides through its enriched base and blood supplementation. It helps cultivate organisms that would otherwise fail to grow on standard nutrient media.
The ability to support such organisms makes it a vital tool in microbiological identification workflows, particularly in cases of severe or difficult-to-diagnose infections.
Antimicrobial Susceptibility Testing Support
Although not typically used as a primary medium for antimicrobial susceptibility testing, Columbia Agar can support such procedures when supplemented appropriately. It is sometimes employed in Streptococcus pyogenes susceptibility testing or for modified disk diffusion techniques, where the visualization of hemolysis enhances interpretive clarity.
Its reliability in supporting pathogen growth ensures reproducible and accurate susceptibility profiles.
Advantages of Columbia Agar
The specific formulation and versatility of Columbia Agar with 5% Sheep Blood offer several practical benefits over other blood agars in diagnostic use.
Enhanced Recovery of Pathogens
Due to its enriched base containing peptones and starch, Columbia Agar can support the growth of even the most nutritionally demanding organisms, ensuring high recovery rates from clinical specimens.
This attribute is crucial when handling polymicrobial infections, where detecting all potential pathogens is essential for effective patient management.
Reliable Hemolysis Visualization
The medium’s ability to clearly display hemolysis types alpha, beta, and gamma allows for accurate differentiation between important clinical pathogens, such as different Streptococcus species, improving the speed and reliability of diagnosis.
This feature makes Columbia Agar particularly valuable in respiratory tract infections, where hemolytic patterns guide immediate empirical therapy decisions.
Versatility in Pathogen Isolation
Columbia Agar’s non-selective nature means it supports the growth of a wide range of gram-positive and gram-negative organisms, making it ideal for use in diverse specimen types. From skin and wound infections to cerebrospinal fluid cultures, it is applicable in almost every clinical setting.
Limitations of Columbia Agar
While highly useful, Columbia Agar with 5% Sheep Blood has some limitations, particularly regarding its selectivity and compatibility with certain pathogens or growth conditions.
Not Selective for Specific Pathogens
Because Columbia Agar is non-selective, it supports the growth of both pathogenic and commensal organisms. In specimens from areas with normal flora (like the throat or skin), overgrowth of non-pathogenic bacteria may obscure the detection of clinically significant pathogens unless selective media are used alongside it.
Limited Use for Anaerobic Cultures Without Modification
Columbia Agar as prepared for routine use is an aerobic medium. Anaerobic pathogens require specific modifications or incubation in anaerobic conditions for optimal growth. While Columbia Agar can be adapted for anaerobes, it is not the first-choice medium unless supplemented with anaerobic growth factors.
Differences Between Columbia Agar and Other Blood Agars
Several types of blood agar exist, each tailored for specific applications or nutritional requirements. This section outlines key differences between Columbia Agar and two other commonly used blood media.
Columbia vs. Blood Agar Base
While both are blood-containing media, Columbia Agar has a more nutritionally enriched base than conventional Blood Agar Base. Columbia’s peptones and starch provide a superior environment for fastidious organisms and produce more distinct hemolysis patterns.
This makes Columbia Agar preferable in situations where detailed hemolytic interpretation or recovery of nutritionally demanding organisms is required.
Columbia vs. Chocolate Agar
Chocolate Agar is prepared by heating blood, which lyses red blood cells and releases intracellular nutrients like hemin and NAD. It supports extremely fastidious organisms such as Neisseria and Haemophilus species, which do not grow well on Columbia Agar with intact red blood cells.
Thus, while Columbia Agar allows observation of hemolysis, Chocolate Agar does not making them complementary but non-interchangeable in diagnostic microbiology.
Recent Developments and Innovations
In recent years, enhanced formulations and new diagnostic approaches have modernized traditional media like Columbia Agar to improve pathogen detection and workflow efficiency.
Chromogenic Modifications
Innovative versions of Columbia Agar incorporate chromogenic substrates that produce color changes in response to specific bacterial enzymes. This allows for simultaneous assessment of hemolysis and preliminary bacterial identification based on colony color.
Such enhancements accelerate diagnostic turnaround times, especially for rapid pathogen identification in high-volume laboratories.
Supplemented Variants for Specialized Pathogens
Modified Columbia Agar formulations now exist, supplemented with selective agents or growth enhancers for particular pathogens. For example, Columbia CNA Agar incorporates antibiotics like colistin and nalidixic acid to inhibit gram-negative bacteria, enhancing the isolation of gram-positive organisms.
These variants extend the utility of Columbia-based media to selective culture applications, particularly in polymicrobial specimen analysis.
Storage and Shelf Life
Proper storage and handling of Columbia Agar are critical for maintaining its sterility, nutritional integrity, and diagnostic performance.
Optimal Storage Conditions
Prepared Columbia Agar plates should be stored at 2–8°C in sealed, moisture-retaining packaging to prevent desiccation. They should be protected from light to preserve blood components and medium clarity.
Shelf Life Guidelines for Prepared Plates
Under optimal conditions, Columbia Agar with 5% Sheep Blood plates typically maintain quality for 4–6 weeks from preparation. Plates should be inspected regularly for contamination, drying, or hemolysis changes before use.
Conclusion
Columbia Agar with 5% Sheep Blood remains a cornerstone medium in clinical bacteriology due to its reliable support for both fastidious and non-fastidious organisms and its ability to differentiate pathogens based on hemolysis. Its enriched formulation and diagnostic versatility have ensured its enduring use in routine practice.
Future trends point toward chromogenic enhancements and pathogen-specific modifications, ensuring this classical medium continues to adapt to modern diagnostic needs. As microbial diagnostics evolve, Columbia Agar remains a vital, trusted tool in medical microbiology.
Frequently Asked Questions (FAQ)
Why is 5% sheep blood specifically used in Columbia Agar?
Sheep blood is preferred because it reliably supports a broad range of pathogens and provides clear, distinguishable hemolysis patterns, making it ideal for clinical diagnostics.
Can Columbia Agar support anaerobic bacteria?
Not in its standard form. It requires anaerobic incubation or modification with additional supplements to support anaerobic pathogens effectively.
What differentiates Columbia Agar from Chocolate Agar?
Columbia Agar uses intact red blood cells, allowing hemolysis observation, while Chocolate Agar contains lysed blood, releasing nutrients for extremely fastidious organisms but does not permit hemolysis detection.
Related Contents
Colony Counter- Types, Principle, Parts, Uses, Examples
Coliform Bacteria- Characteristics, Examples, Identification