Introduction
Coccidioidomycosis (pronounced kok-sid-ee-oy-doh-my-KOH-sis) is a fungal infection caused by Coccidioides species. It is also commonly known as “Valley Fever” because it is most prevalent in the valleys of the southwestern United States, especially in California and Arizona. People usually get infected by breathing in spores from the air—not from contact with sick people or animals.
Although many people recover without needing treatment, coccidioidomycosis can sometimes become serious—especially in people with weak immune systems.
This article provides a simple, clear, and complete overview of this disease, from what causes it to how it is diagnosed, treated, and prevented.
Table of Contents
What Causes Coccidioidomycosis?
The infection is caused by two related fungi:
- Coccidioides immitis
- Coccidioides posadasii
These fungi live in soil, especially in dry, dusty, and hot regions. They form spores (called arthroconidia) that can be easily carried in the air when the soil is disturbed—by wind, farming, construction, or digging.
When people inhale these spores, the fungus enters the lungs and can cause illness.
Where Is It Found? (Geographic Distribution)
Coccidioidomycosis is endemic (commonly found) in certain parts of the Americas. Major endemic areas include:
- Southwestern United States:
- Arizona
- California (Central Valley)
- New Mexico
- Texas
- Nevada
- Utah
- Northern Mexico
- Parts of Central and South America (e.g., Argentina, Brazil, Paraguay)
It is most common in desert regions with hot summers and mild winters.
How Does It Spread?
Not contagious – Coccidioidomycosis does not spread from person to person.
Infection occurs by:
- Inhaling airborne fungal spores
- Exposure to disturbed soil (farming, construction work, dust storms)
Rarely, the fungus can enter through the skin or be spread via organ transplants or laboratory accidents.
Who is at Risk?
Anyone living or traveling in endemic areas can get infected, but certain groups are more vulnerable:
Higher Risk Groups:
- Farmers, construction workers, archaeologists (exposed to soil)
- People with weak immune systems (HIV/AIDS, cancer patients, organ transplant recipients)
- Pregnant women, especially in the 3rd trimester
- Elderly people
- People of African-American, Filipino, or Hispanic descent (for unknown genetic reasons)
How Does It Affect the Body? (Pathogenesis)
After inhaling fungal spores:
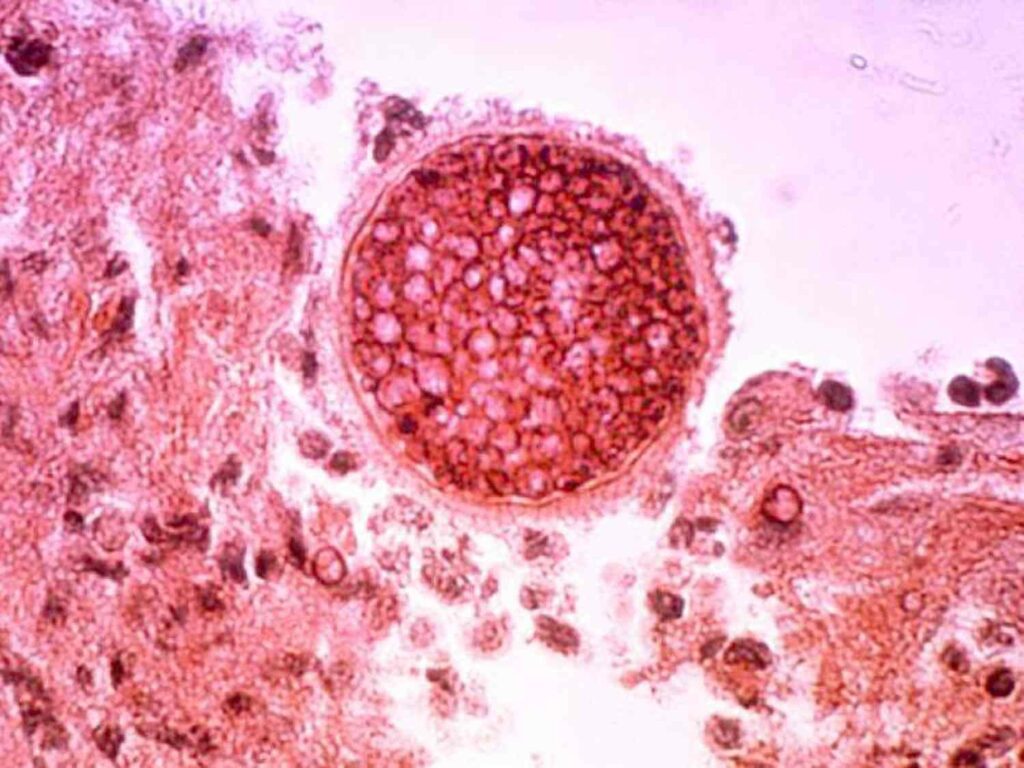
- Spores lodge in the lungs and change into spherules.
- Spherules grow and release endospores.
- The cycle continues, causing local infection or sometimes spreading to other organs.
The body’s immune system may:
- Fight off the infection with no symptoms.
- Cause mild to severe symptoms (flu-like).
- Fail to contain it, leading to chronic or disseminated disease.
Types of Coccidioidomycosis
There are three main forms:
1. Acute (Primary Pulmonary) Coccidioidomycosis
- Most common
- Occurs after inhalation of spores
- Usually mild or asymptomatic
- Flu-like symptoms appear 1–3 weeks after exposure
2. Chronic Pulmonary Coccidioidomycosis
- Happens when the acute form doesn’t resolve
- Can mimic tuberculosis
- Symptoms can last months or years
3. Disseminated Coccidioidomycosis
- Most serious form
- The fungus spreads to skin, bones, joints, or brain
- Life-threatening if not treated
- More common in immunocompromised people
Signs and Symptoms
Acute Infection Symptoms (like flu):
- Fever
- Cough
- Chest pain (sharp or dull)
- Shortness of breath
- Fatigue
- Night sweats
- Joint and muscle pain
- Headache
- Rash (erythema nodosum: red, painful bumps on legs)
Chronic Infection:
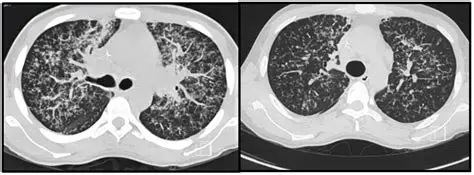
- Persistent cough
- Weight loss
- Blood in sputum
- Fatigue
- Lung nodules or cavities (seen in X-rays)
Disseminated Infection:
- Skin ulcers or nodules
- Swollen joints (arthritis-like symptoms)
- Bone pain
- Meningitis (headache, neck stiffness, confusion)
- Brain or spinal cord involvement
Diagnosis
Because the symptoms are similar to many other conditions (like the flu or TB), coccidioidomycosis is often misdiagnosed or overlooked.
Diagnostic Tools:
- History and Exposure
- Recent travel to or residence in endemic areas
- Dust exposure
- Blood Tests (Serology)
- Detect antibodies (IgM, IgG) against Coccidioides
- Most common initial test
- Sputum or Tissue Culture
- Identifies the fungus from lungs or infected sites
- Risky due to aerosol spread—done in special labs
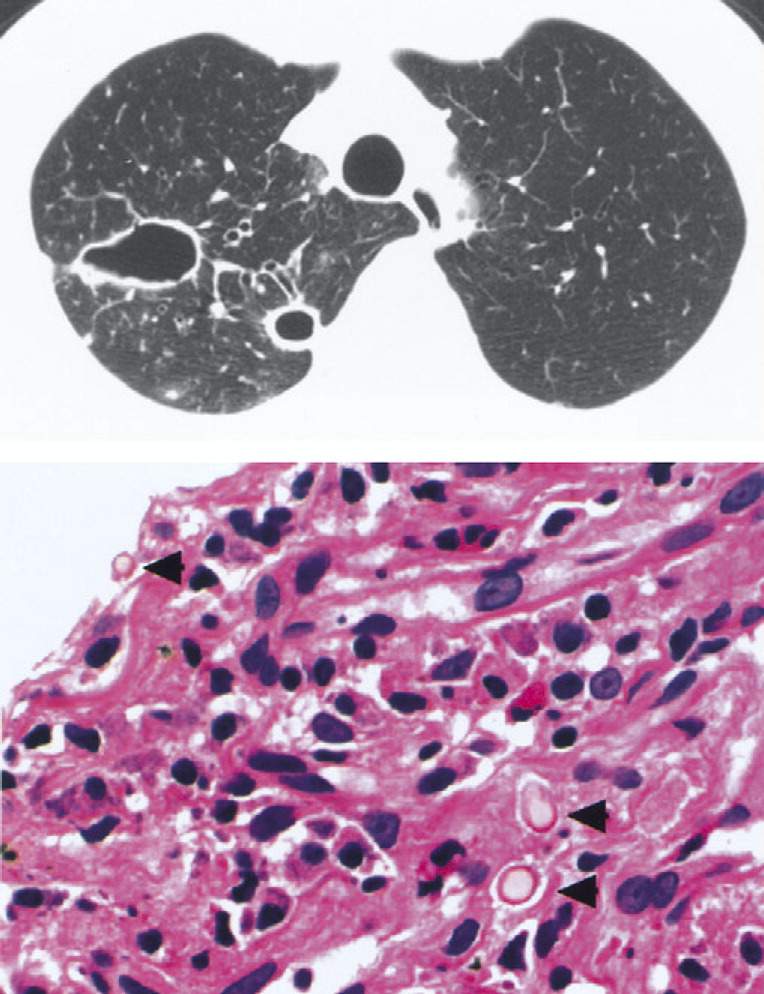
- Microscopy
- Shows spherules in tissue or sputum
- Chest X-ray / CT Scan
- Reveals nodules, cavities, or infiltrates
- Biopsy
- May be needed for deep or unusual infections
Treatment
Many people recover without treatment, especially if symptoms are mild. However, treatment is essential in moderate, chronic, or disseminated cases.
Antifungal Medications:
1. Fluconazole (oral)
- Most commonly used
- Especially for mild to moderate disease or meningitis
2. Itraconazole
Alternative to fluconazole
3. Amphotericin B (IV)
- For severe or life-threatening cases
- More side effects
Duration of Treatment:
- Mild cases: weeks to a few months
- Severe cases: 6 months to 1 year or longer
- Meningitis: may require lifelong therapy
Recovery and Prognosis
- Most people recover fully without complications.
- Symptoms may persist for weeks or months even after the infection clears.
- Relapse is possible in immunocompromised individuals.
Prevention Tips
There’s no vaccine yet, but the following can help reduce risk:
Personal Precautions:
- Avoid digging or exposure to dusty soil in endemic areas.
- Wear masks during outdoor work or dust storms.
- Keep windows closed during dusty weather.
- Wet soil before working to reduce dust.
For Vulnerable Individuals:
- Extra caution if immunosuppressed or pregnant
- Limit travel to endemic areas if possible
- Regular checkups and blood tests if exposure is known
Interesting Facts
- 60% of infected people have no symptoms.
- Sometimes called the “Great Imitator” because it mimics flu, TB, or pneumonia.
- First discovered in Argentina in 1892.
- There are occasional outbreaks after earthquakes or dust storms.
- One of the few fungal infections that can spread through organ transplantation.
Differential Diagnosis (Conditions That Mimic BV)
Doctors may initially mistake coccidioidomycosis for:
- Influenza
- Community-acquired pneumonia
- Tuberculosis
- COVID-19
- Lung cancer
- Sarcoidosis
That’s why travel history and proper testing are so important.
Conclusion
Coccidioidomycosis, or Valley Fever, is a fungal disease that mainly affects the lungs but can also spread throughout the body in serious cases. It is not contagious, and many people recover without needing medication. But for others—especially those with weak immunity—it can be chronic or life-threatening.
The key to managing coccidioidomycosis lies in:
- Early recognition of symptoms
- Understanding your exposure risks
- Timely diagnosis and treatment
With proper care, most people make a full recovery. For those in high-risk areas or groups, awareness and prevention are the best tools for staying safe.
FREQUENTLY ASKED QUESTIONS
What is coccidioidomycosis?
Coccidioidomycosis, also called Valley Fever, is a fungal infection caused by breathing in spores of Coccidioides species—fungi that live in dry, dusty soil, especially in the southwestern U.S. and parts of Latin America.
What causes it?
It is caused by inhaling airborne spores of Coccidioides immitis or Coccidioides posadasii, usually from disturbed soil (e.g., farming, digging, windstorms).
Is Valley Fever contagious?
No. Coccidioidomycosis does not spread from person to person.
It is only acquired by inhaling fungal spores from the environment.
Related Articles