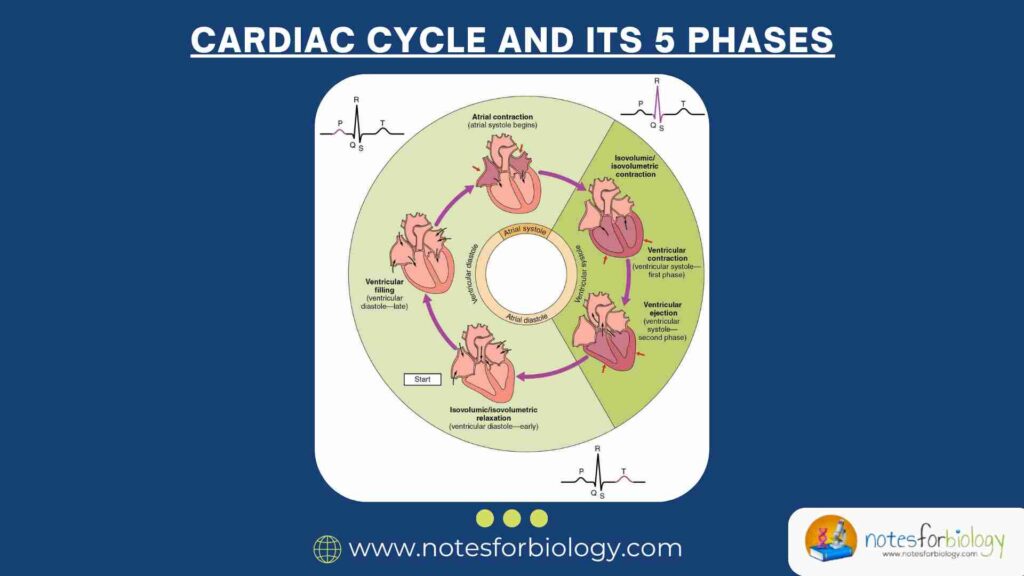
Definition of the Cardiac Cycle
The cardiac cycle refers to the complete sequence of electrical and mechanical events that occur from the beginning of one heartbeat to the beginning of the next. This intricate process ensures the continuous circulation of blood throughout the body, delivering oxygen and nutrients while removing waste products. Lasting approximately 0.8 seconds in a healthy adult at rest, the cardiac cycle consists of five distinct phases that alternate between periods of contraction (systole) and relaxation (diastole). Each phase is precisely coordinated by the heart’s conduction system and results in the characteristic “lub-dub” sounds heard through a stethoscope.
Summary of Cardiac Cycle
- The cardiac cycle is the rhythmic sequence of heart contractions and relaxations that pump blood throughout the body.
- It consists of systole (contraction), which pushes blood out, and diastole (relaxation), which refills the heart chambers.
- This continuous cycle keeps oxygen-rich blood flowing, ensuring the body stays energized and alive.
Table of Contents
5 Phases of Cardiac Cycle
Phase 1: Atrial Contraction (Late Diastole)
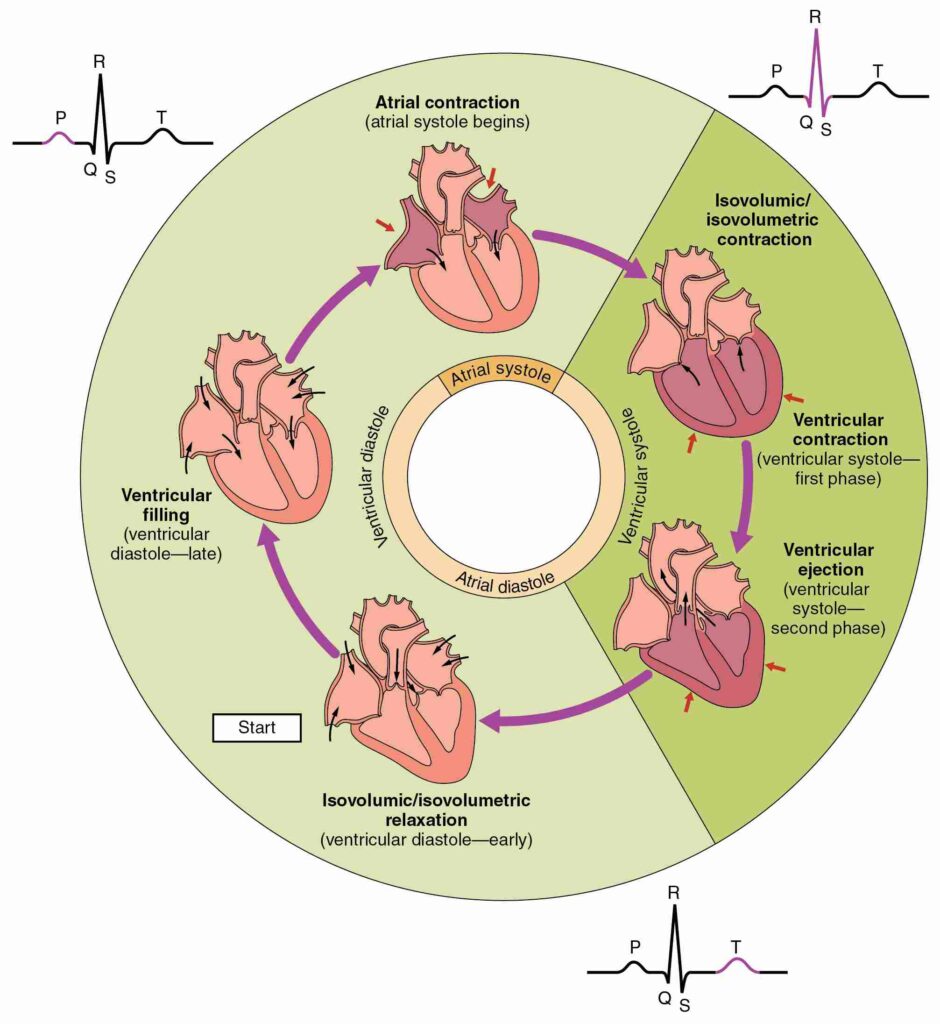
The cardiac cycle begins with atrial contraction, also known as atrial systole or the “atrial kick.” This phase represents the final stage of ventricular filling before the ventricles themselves contract.
During this phase, the sinoatrial (SA) node the heart’s natural pacemaker initiates an electrical impulse that spreads across both atria, causing them to contract. This contraction forces approximately 25% of the remaining blood into the ventricles, adding to the 75% that passively filled during earlier relaxation. The atrioventricular (AV) valves (tricuspid and mitral) remain open during this phase, while the semilunar valves (aortic and pulmonary) stay closed to prevent backflow.
Pressure changes during atrial contraction are relatively small compared to ventricular systole, typically rising only 5-10 mmHg in the atria. On an electrocardiogram (ECG), this phase correlates with the P wave, which represents atrial depolarization. In some individuals, a faint fourth heart sound (S4) may be audible during this phase, though its presence in adults usually indicates abnormal ventricular stiffness.
The importance of this phase becomes evident in conditions like atrial fibrillation, where ineffective atrial contractions can reduce cardiac output by up to 20%. This demonstrates how even this brief period significantly contributes to the heart’s pumping efficiency.
Phase 2: Isovolumetric Contraction (Early Systole)
The isovolumetric contraction phase marks the beginning of ventricular systole, where the ventricles contract without changing volume as all heart valves remain closed.
Following atrial contraction, the electrical impulse reaches the atrioventricular node and then rapidly spreads through the bundle of His and Purkinje fibers, triggering ventricular contraction. As pressure builds within the ventricles, it quickly surpasses atrial pressure, causing the AV valves to snap shut producing the first heart sound (S1 or “lub”).
During this 50-100 millisecond phase:
- Ventricular pressure rises sharply (from ≈10 mmHg to ≈80 mmHg in the left ventricle)
- No blood exits the heart yet (hence “isovolumetric”)
- The ECG shows the QRS complex (ventricular depolarization)
This phase is crucial for building sufficient pressure to open the semilunar valves. Any prolongation (e.g., in aortic stenosis) reduces cardiac efficiency and can lead to pathological S1 splitting.
Phase 3: Rapid Ejection (Mid-Systole)
The rapid ejection phase occurs when ventricular pressure exceeds arterial pressure, forcing open the semilunar valves and propelling blood into circulation.
Once ventricular pressure surpasses aortic (≈80 mmHg) and pulmonary (≈8 mmHg) pressures:
- The aortic and pulmonary valves open abruptly
- ≈70% of stroke volume is ejected within the first third of systole
- Left ventricular pressure peaks at 120 mmHg
This phase creates the arterial pulse we feel at the wrist. The heart’s twisting motion during contraction (like wringing a towel) enhances ejection efficiency. Coronary blood flow is minimal here due to compressed coronary arteries.
Phase 4: Reduced Ejection (Late Systole)
As ventricular contraction wanes, blood flow slows until pressures equalize, marking the end of systole.
During this brief period:
- The remaining 30% of stroke volume exits more slowly
- Ventricular repolarization begins (T wave on ECG)
- Semilunar valves start drifting closed as flow diminishes
This phase is vulnerable to arrhythmias that can disrupt the transition to relaxation.
Phase 5: Isovolumetric Relaxation (Early Diastole)
All valves close again as ventricles relax before refilling begins.
Key events:
- Ventricular pressure falls below arterial pressure → semilunar valves close (S2/”dub”)
- Brief period where all valves are closed (protects ventricles from backflow)
- Atria begin refilling passively
This phase is critical for coronary perfusion, as the relaxed ventricles no longer compress coronary arteries.
Conclusion: The Symphony of Life
The cardiac cycle represents one of nature’s most exquisite biological mechanisms—a self-regulating, rhythmically precise process that sustains life from before birth until our final moment. Each phase demonstrates remarkable engineering: from the atrial kick’s efficiency boost to the power-generating isovolumetric contraction, from the forceful ejection that creates our pulse to the protective valve closures during relaxation.
Understanding these phases illuminates how exercise enhances cardiac output (via increased rate and contractility), why valve disorders cause characteristic murmurs, and how arrhythmias disrupt this delicate timing. Modern cardiology interventions—from pacemakers to valve replacements—all aim to restore or optimize this fundamental cycle.
As research continues to unravel the molecular mechanisms underlying each phase, we gain not only deeper appreciation for this vital process but also new avenues for treating cardiovascular diseases that remain humanity’s leading cause of mortality. The cardiac cycle, in its elegant simplicity and complexity, truly embodies the ceaseless rhythm of life itself.
Frequently Asked Questions (FAQs)
What is the cardiac cycle?
The cardiac cycle refers to the sequence of events in the heart from the start of one heartbeat to the beginning of the next. It includes the contraction (systole) and relaxation (diastole) phases of the atria and ventricles, ensuring continuous blood circulation throughout the body.
What are the main phases of the cardiac cycle?
The cardiac cycle comprises several phases:
Atrial systole: Atria contract, pushing blood into the ventricles.
Isovolumetric contraction: Ventricles begin to contract with all valves closed.
Ventricular ejection: Semilunar valves open; blood is pumped into the arteries.
Isovolumetric relaxation: Ventricles relax with all valves closed.
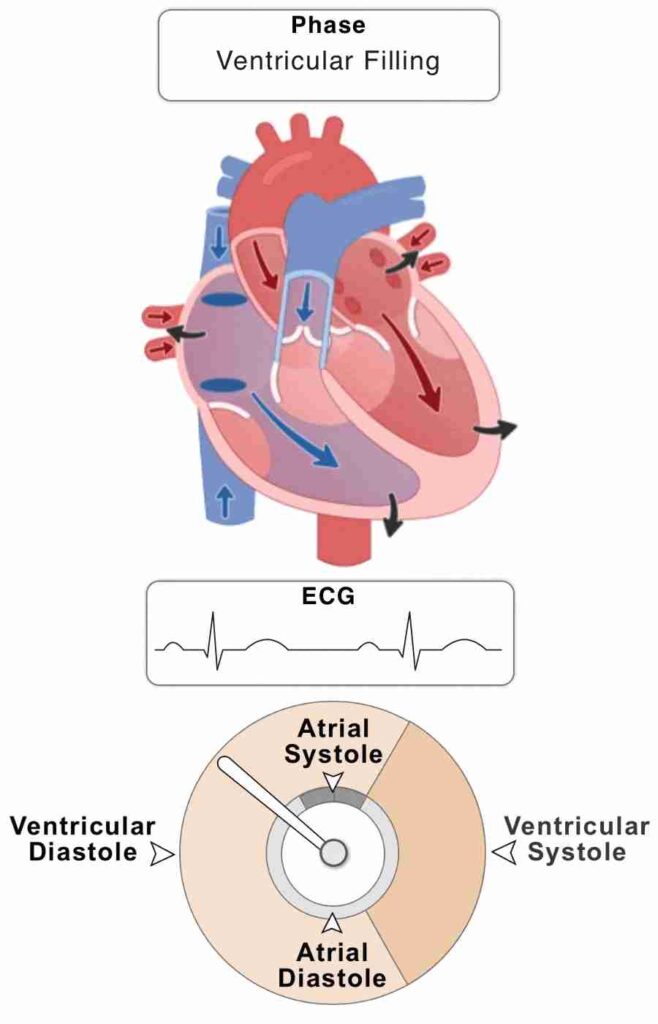
Ventricular filling: AV valves open; ventricles fill with blood.
What causes the “lub-dub” sounds of the heartbeat?
The “lub” (first heart sound) occurs when the atrioventricular (AV) valves close at the beginning of ventricular systole. The “dub” (second heart sound) happens when the semilunar valves close at the start of ventricular diastole.
Related Articles