What is Carbapenemases?
Carbapenemases are a subset of β-lactamase enzymes produced by certain bacteria, granting them resistance to carbapenems—a class of antibiotics often reserved as a last resort for treating severe bacterial infections. These enzymes hydrolyze the β-lactam ring present in carbapenem antibiotics, rendering them ineffective. The emergence and spread of carbapenemase-producing organisms have become a significant concern in healthcare settings due to limited treatment options and increased morbidity and mortality rates.
Summary of Carbapenemases
- Carbapenemases are enzymes produced by certain bacteria that break down carbapenem antibiotics, rendering them ineffective against infections.
- These enzymes are categorized into classes A, B, and D, including types like KPC, NDM, and OXA-48, and are often found in bacteria such as Klebsiella pneumoniae and Escherichia coli.
- The emergence of carbapenemase-producing bacteria poses a significant public health challenge due to limited treatment options and increased risk of severe infections, especially in healthcare settings.
Table of Contents
Types of Carbapenemases
Carbapenemases are categorized based on the Ambler classification system into three primary classes: A, B, and D.
Class A: Serine β-lactamases
These enzymes utilize a serine residue in their active site to hydrolyze β-lactam antibiotics. Notable examples include:
Klebsiella pneumoniae carbapenemase (KPC): First identified in the United States, KPC enzymes have since been detected worldwide and are commonly found in Enterobacteriaceae.
Serratia marcescens enzyme (SME): Primarily found in Serratia marcescens, SME enzymes are less prevalent but still pose a threat due to their resistance capabilities.
Not metalloenzyme carbapenemase/Imipenem-hydrolyzing β-lactamase (NMC-A/IMI): These enzymes are less commonly encountered but contribute to carbapenem resistance in certain bacterial strains.
Class B: Metallo-β-lactamases (MBLs)
Class B carbapenemases require divalent metal ions, typically zinc, for their enzymatic activity. They are not inhibited by traditional β-lactamase inhibitors. Key examples include:
New Delhi metallo-β-lactamase (NDM): First identified in 2008, NDM enzymes have rapidly spread globally, often found in Enterobacteriaceae and Acinetobacter species.
Verona integron-encoded metallo-β-lactamase (VIM): Initially discovered in Italy, VIM enzymes are now widespread and found in various Gram-negative bacteria.
Imipenemase (IMP): First reported in Japan, IMP enzymes have been identified in multiple countries and are associated with resistance in Pseudomonas and Acinetobacter species.
Class D: Oxacillinase-type β-lactamases
Class D enzymes, also known as oxacillinases, possess a serine-based mechanism but differ structurally from Class A enzymes. Significant examples include:
OXA-48-like enzymes: Predominantly found in Enterobacteriaceae, especially Klebsiella pneumoniae, these enzymes are notable for their ability to hydrolyze penicillins and carbapenems but have limited activity against extended-spectrum cephalosporins.
Significance of Carbapenemases
The emergence of carbapenemase-producing organisms (CPOs) has profound implications for public health,
Limited Treatment Options: Carbapenemases confer resistance to a broad range of β-lactam antibiotics, including carbapenems, often leaving few effective treatment alternatives.
High Mortality Rates: Infections caused by CPOs are associated with increased morbidity and mortality, particularly in vulnerable populations such as hospitalized patients.
Rapid Dissemination: Carbapenemase genes are often located on mobile genetic elements like plasmids, facilitating horizontal gene transfer among bacteria and accelerating the spread of resistance.
Diagnostic Challenges: Detecting carbapenemase production can be complex, requiring specialized laboratory tests, which may delay appropriate treatment and infection control measures.
Associated Bacteria of Carbapenemases
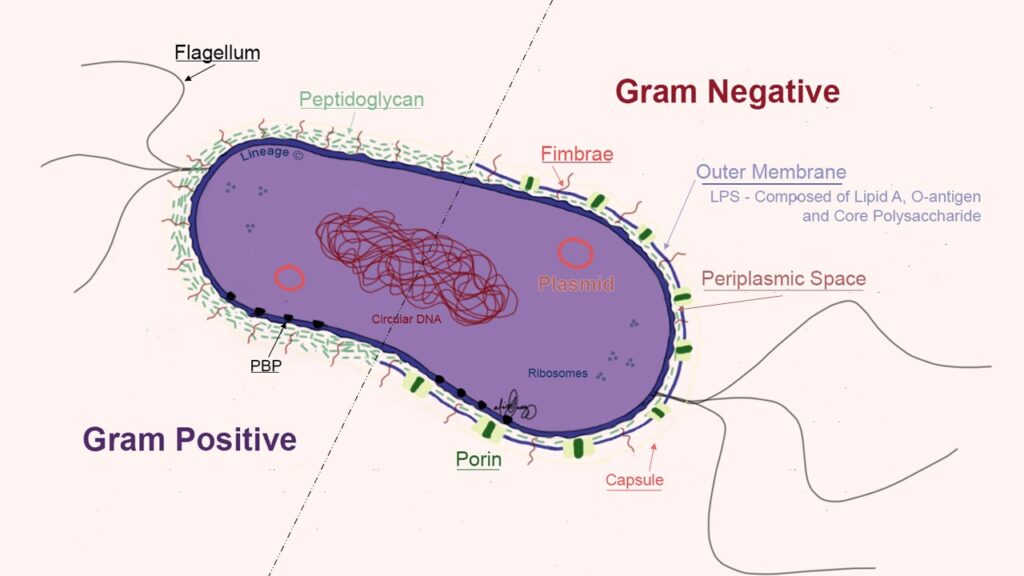
Several Gram-negative bacteria have been identified as carriers of carbapenemase enzymes:
Enterobacteriaceae Family: Includes common pathogens such as Klebsiella pneumoniae, Escherichia coli, and Enterobacter species.
Pseudomonas aeruginosa: A non-fermenting Gram-negative bacterium known for its intrinsic resistance mechanisms and ability to acquire carbapenemase genes.
Acinetobacter baumannii: Another non-fermenter associated with hospital-acquired infections and notable for its capacity to harbor various resistance determinants, including carbapenemases.
Conclusion
Carbapenemases represent a formidable challenge in the fight against antimicrobial resistance. Their ability to inactivate a broad spectrum of β-lactam antibiotics, coupled with the ease of gene transfer among bacteria, underscores the urgency for vigilant surveillance, robust infection control practices, and the development of novel therapeutic agents. Addressing the threat posed by carbapenemase-producing organisms requires a coordinated global effort encompassing healthcare providers, microbiologists, researchers, and policymakers.
Frequently Asked Questions ( FAQs)
What is klebsiella pneumoniae carbapenemase?
KPC is a superbug enzyme that destroys powerful antibiotics like carbapenems, making infections nearly untreatable. First found in 1996, it spreads easily in hospitals through bacteria’s shared DNA, causing deadly bloodstream, lung, and urinary infections. Detecting KPC requires special lab tests, and its global spread makes it a critical health threat needing strict hospital controls.
What are the treatment for KPC infections?
Treatment options for KPC infections are limited but may include:
Ceftazidime-avibactam: A combination antibiotic effective against many KPC-producing bacteria.
Meropenem-vaborbactam: Another combination therapy targeting KPC-producing organisms.
Colistin: Used as a last-resort option due to its potential toxicity.
How is KPC detected in laboratory settings?
KPC can be identified through laboratory tests such as:
Phenotypic tests: These detect carbapenemase production by observing bacterial growth patterns.
Molecular tests: These identify specific resistance genes, including KPC, using techniques like PCR.
Both methods are crucial for accurate diagnosis and appropriate treatment planning.
Related Articles

