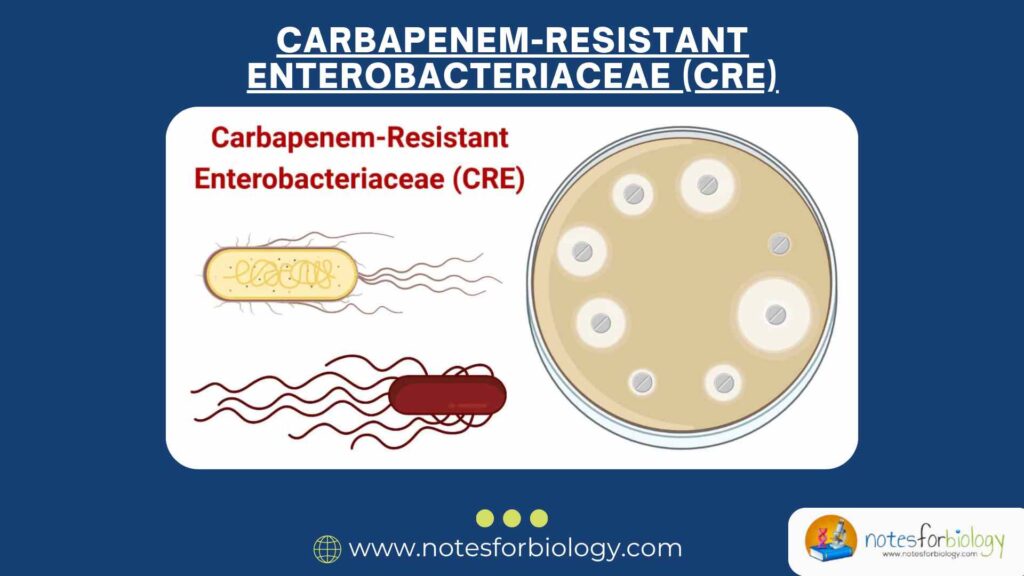
What is Carbapenem-Resistant Enterobacteriaceae (CRE)?
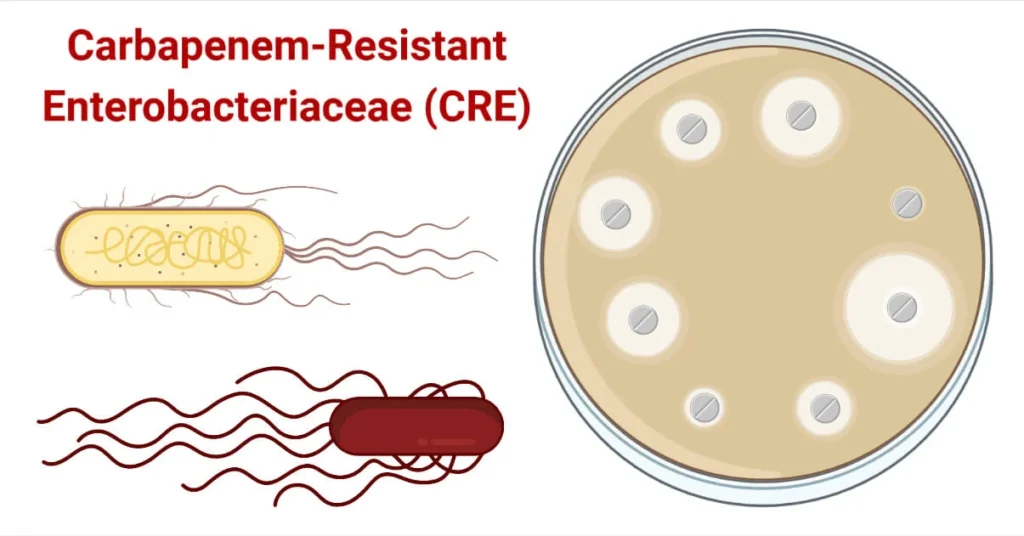
Carbapenem-Resistant Enterobacteriaceae (CRE) are a group of Gram-negative bacteria that have developed resistance to carbapenem antibiotics, which are often considered the last line of defense against severe bacterial infections. These bacteria, including common species like Escherichia coli and Klebsiella pneumoniae, are part of the Enterobacteriaceae family and are typically found in the human gut. While many Enterobacteriaceae are harmless, CRE strains can cause serious infections, especially in healthcare settings. The resistance to carbapenems makes these infections particularly challenging to treat, leading to higher morbidity and mortality rates.
Summary of Carbapenem-Resistant Enterobacteriaceae
- CRE are dangerous bacteria resistant to powerful antibiotics, making infections hard to treat and potentially life-threatening.
- CRE are multidrug-resistant gram-negative bacteria producing carbapenemases, posing significant challenges in clinical management and infection control.
- CRE represents a growing public health threat due to its high resistance to antibiotics and potential for rapid spread in healthcare settings.
Table of Contents
2. Epidemiology of Carbapenem-Resistant Enterobacteriaceae
Global Spread
CRE infections have been reported worldwide, with varying prevalence across regions. In the United States, for instance, the Centers for Disease Control and Prevention (CDC) reported that in 2017, CRE caused approximately 13,100 infections in hospitalized patients, resulting in about 1,100 deaths. The spread of CRE is not confined to hospitals; community settings have also seen cases, indicating a broader dissemination.
Risk Factors
Several factors increase the risk of acquiring a CRE infection:
- Healthcare Exposure: Patients in hospitals or long-term care facilities are at higher risk, especially those with prolonged stays.
- Medical Devices: Use of devices like ventilators, urinary catheters, or intravenous catheters can facilitate infection.
- Antibiotic Usage: Prior or prolonged use of antibiotics, particularly carbapenems, can disrupt normal flora and promote resistance.
- Weakened Immune Systems: Individuals with compromised immunity, such as the elderly or those with chronic illnesses, are more susceptible.
3. Mechanisms of Resistance
CRE bacteria employ various mechanisms to resist carbapenem antibiotics:
Carbapenemase Production
The primary mechanism is the production of enzymes called carbapenemases, which break down carbapenem antibiotics, rendering them ineffective. Notable carbapenemases include:
- KPC (Klebsiella pneumoniae carbapenemase): Common in the U.S. and other regions.
- NDM (New Delhi metallo-β-lactamase): First identified in India, now widespread globally.
- OXA-48-like enzymes: Found in parts of Europe, North Africa, and the Middle East.
Porin Channel Alterations
Changes or loss of porin proteins in the bacterial outer membrane can reduce antibiotic uptake, contributing to resistance.
Efflux Pumps
Overexpression of efflux pumps can expel antibiotics from bacterial cells before they can act.
Horizontal Gene Transfer
Resistance genes can be transferred between bacteria via plasmids, facilitating rapid spread of resistance traits.
4. Clinical Manifestations of Carbapenem-Resistant Enterobacteriaceae
CRE can cause a range of infections, often depending on the site of entry and patient vulnerability:
- Urinary Tract Infections (UTIs): Symptoms include frequent urination, burning sensation, and urgency.
- Pneumonia: Characterized by cough, fever, and difficulty breathing.
- Bloodstream Infections (Sepsis): Presents with fever, chills, low blood pressure, and organ dysfunction.
- Wound Infections: Redness, swelling, and pus at the infection site.
- Meningitis: Though rare, CRE can cause infections in the central nervous system.
- Asymptomatic Colonization: Individuals can carry CRE without showing symptoms, posing a risk of transmission.
5. Diagnosis of Carbapenem-Resistant Enterobacteriaceae
Accurate and timely diagnosis is crucial for managing CRE infections:
Culture and Sensitivity Testing
Samples from blood, urine, or other infected sites are cultured to identify the bacteria and determine antibiotic susceptibility.
Molecular Methods
Polymerase Chain Reaction (PCR) and other molecular techniques can detect specific resistance genes like blaKPC, blaNDM, and blaOXA-48.
Screening
Rectal swabs may be used to identify asymptomatic carriers, especially in outbreak settings.
6. Treatment Options of Carbapenem-Resistant Enterobacteriaceae
Treating CRE infections is challenging due to limited effective antibiotics:
Limited Antibiotics
Options include older antibiotics like polymyxins (e.g., colistin) and tigecycline, though they may have significant side effects.
Combination Therapy
Using multiple antibiotics may be more effective than monotherapy, though evidence varies.
Newer Agents
Drugs like ceftazidime-avibactam and meropenem-vaborbactam show promise against certain CRE strains.
Supportive Care
Includes fluid management, oxygen therapy, and other measures to support vital functions.
7. Prevention and Control of Carbapenem-Resistant Enterobacteriaceae
Preventing CRE infections involves multiple strategies:
Infection Control Practices
Strict hand hygiene, use of personal protective equipment, and environmental cleaning in healthcare settings.
Antimicrobial Stewardship
Prudent use of antibiotics to minimize the development of resistance.
Surveillance
Monitoring and reporting CRE cases to detect and manage outbreaks promptly.
Education
Training healthcare workers and informing the public about CRE risks and prevention strategies.
8. Public Health Implications
CRE infections have significant implications:
- High Mortality Rates: Infections caused by CRE can have mortality rates as high as 40–50%, especially in bloodstream infections.
- Economic Impact: Infections lead to longer hospital stays and increased healthcare costs.
- Research and Development: Urgent need for new antibiotics and diagnostic tools to combat CRE.
- Global Health Threat: CRE represents a significant challenge to modern medicine due to limited treatment options and high mortality rates.
9. Conclusion
Carbapenem-Resistant Enterobacteriaceae are formidable pathogens that compromise the effectiveness of last-resort antibiotics. Combating CRE requires a multifaceted approach, including stringent infection control, responsible antibiotic use, ongoing surveillance, and investment in research for new therapeutic options.
Frequently Asked Questions (FAQs)
What are the symptoms of CRE infections?
Carbapenem-Resistant Enterobacteriaceae (CRE) infections can present with various symptoms, depending on the part of the body affected. Common signs include fever, chills, and fatigue. If the lungs are involved, symptoms may encompass coughing and shortness of breath. Urinary tract infections caused by CRE can lead to pain or burning during urination, increased frequency, and urgency. Wound infections might exhibit redness, swelling, and pus. In severe cases, such as bloodstream infections or meningitis, individuals may experience more serious symptoms like confusion, stiff neck, or sensitivity to light. It’s also important to note that some people can carry CRE bacteria without showing any symptoms, a condition known as colonization.
How is a CRE infections diagnosed?
Diagnosing a CRE infection involves several steps. Healthcare providers will start by reviewing your medical history and conducting a physical examination. They may order laboratory tests, such as blood, urine, or sputum cultures, to identify the presence of bacteria. Once the bacteria are identified, further tests determine if they are resistant to carbapenem antibiotics. Imaging studies like chest X-rays might be used if a lung infection is suspected. In some cases, molecular tests can detect specific resistance genes. These diagnostic procedures help in confirming the infection and guiding appropriate treatment.
What treatments are available for CRE infections?
Treatments that are available for CRE infections are
Search Volume: Approximately 1,100 searches per month
Keyword Difficulty: Low (KD ~14)
Related Articles