In the evolving landscape of infectious diseases, antibiotic-resistant bacteria have emerged as significant threats to public health systems worldwide. Among them, Acinetobacter baumannii has gained notoriety for its remarkable ability to develop resistance to multiple antibiotics, including carbapenems, which are often considered drugs of last resort.
Carbapenem-Resistant Acinetobacter baumannii (CRAB) poses a serious challenge in healthcare settings, particularly in intensive care units (ICUs), post-surgical wards, and long-term care facilities. The organism’s resilience in adverse environmental conditions and its multidrug-resistant (MDR) nature contribute to prolonged hospital outbreaks, high morbidity, and elevated mortality rates.
Summary of Carbapenem-Resistant Acinetobacter baumannii (CRAB)
- Carbapenem-Resistant Acinetobacter baumannii (CRAB) is a highly drug-resistant hospital pathogen causing severe infections like pneumonia, bloodstream, urinary, and wound infections, especially in critically ill patients.
- Its resistance to carbapenems is driven by carbapenemases, efflux pumps, and porin loss, leaving treatment options very limited, often requiring last-resort drugs.
- Control relies on strict infection measures, rapid molecular diagnostics, active surveillance, and urgent development of new antimicrobial therapies.
Table of Contents
What is Acinetobacter baumannii?
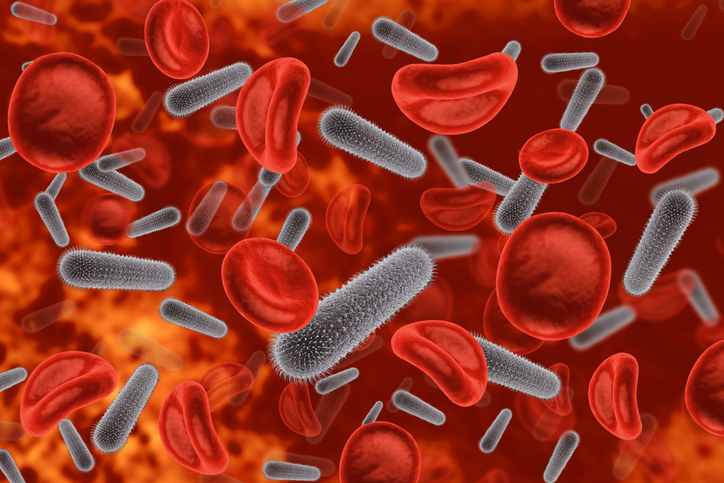
To appreciate the significance of CRAB, it is first essential to understand the biological characteristics of its progenitor, Acinetobacter baumannii. This bacterium belongs to the family Moraxellaceae and is a strictly aerobic, gram-negative, non-motile, catalase-positive coccobacillus. It is naturally found in water and soil but has increasingly become adapted to hospital environments where it can persist for extended periods on inanimate surfaces.
This environmental persistence enables it to survive in healthcare settings, where it opportunistically infects vulnerable individuals. Its typical targets include patients with compromised immune systems, those receiving mechanical ventilation, and individuals undergoing invasive procedures such as catheterization or surgery.
Definition of Carbapenem-Resistant Acinetobacter baumannii
Carbapenem-Resistant Acinetobacter baumannii, commonly abbreviated as CRAB, refers to strains of A. baumannii that exhibit resistance to carbapenem antibiotics, which include imipenem, meropenem, doripenem, and ertapenem. These antibiotics belong to the β-lactam class and are valued for their broad-spectrum activity against gram-negative bacteria.
Carbapenem-Resistant Acinetobacter baumannii (CRAB) strains often display multidrug resistance, which limits treatment options and contributes to difficult-to-control nosocomial outbreaks. Infections caused by CRAB are associated with increased morbidity, prolonged hospital stays, higher healthcare costs, and elevated mortality rates, particularly in critically ill patients.
Epidemiology of Carbapenem-Resistant Acinetobacter baumannii Infections
Over the past two decades, Carbapenem-Resistant Acinetobacter baumannii (CRAB) has emerged as a prominent cause of hospital-acquired infections, with increasing prevalence across continents. The incidence of CRAB is especially high in Asia, the Mediterranean, the Middle East, and parts of South America.
CRAB outbreaks are frequently reported in ICUs, where patients are often immunocompromised and subjected to invasive devices such as endotracheal tubes and central venous catheters. The bacterium’s ability to survive desiccation and resist disinfectants allows it to persist on hospital equipment, bed rails, and other environmental surfaces, facilitating its spread from patient to patient through direct or indirect contact.
In 2017, the World Health Organization (WHO) categorized CRAB as a Critical Priority Pathogen, underscoring the urgent need for the development of new antimicrobials and infection control strategies.
Mechanisms of Carbapenem Resistance
The development of carbapenem resistance in A. baumannii is attributed to a combination of several molecular mechanisms. These mechanisms either destroy the antibiotic, reduce its access to bacterial targets, or actively pump the antibiotic out of the cell.
Production of Carbapenemases
The most significant resistance mechanism is the production of enzymes known as carbapenemases. These enzymes degrade the β-lactam ring present in carbapenem molecules, thereby neutralizing the antibiotic’s activity. In A. baumannii, carbapenemases are predominantly of the OXA-type (class D β-lactamases). Common examples include OXA-23, OXA-24/40, OXA-58, and the chromosomally encoded OXA-51-like enzymes.
Among these, OXA-23 is the most widely disseminated carbapenemase globally, often located on mobile genetic elements such as plasmids and transposons, which facilitate horizontal gene transfer.
Efflux Pump Overexpression
Efflux pumps are membrane proteins that actively extrude toxic substances, including antibiotics, from the bacterial cell. In CRAB, overexpression of efflux pump systems, particularly the AdeABC, AdeIJK, and AdeFGH pumps, contributes to multidrug resistance. These pumps reduce intracellular concentrations of carbapenems and other antibiotics, diminishing their therapeutic effectiveness.
Porin Channel Alterations
Carbapenem antibiotics typically enter gram-negative bacteria through outer membrane porins. In CRAB, mutations or downregulation of these porin proteins, such as CarO, restrict antibiotic uptake. This decreased permeability is a crucial contributor to carbapenem resistance, especially when combined with other mechanisms like carbapenemase production.
Target Site Modification
Though relatively rare in A. baumannii, carbapenem resistance can also arise from modifications in penicillin-binding proteins (PBPs), which are the target enzymes of β-lactam antibiotics. Mutations in PBPs can reduce the binding affinity of carbapenems, rendering them ineffective.
Clinical Manifestations of Carbapenem-Resistant Acinetobacter baumannii (CRAB) Infections
Carbapenem-Resistant Acinetobacter baumannii (CRAB) is an opportunistic pathogen responsible for a wide range of hospital-acquired infections, often in critically ill and immunocompromised patients. The clinical outcomes of these infections are typically severe due to limited treatment options and the organism’s multidrug-resistant nature.
Hospital-Acquired Pneumonia (HAP) and Ventilator-Associated Pneumonia (VAP)
The most common and serious infections caused by CRAB are respiratory tract infections, particularly ventilator-associated pneumonia. These infections are difficult to treat, often requiring mechanical ventilation and aggressive antibiotic therapy. Symptoms include fever, productive cough, hypoxia, and chest infiltrates visible on radiography.
Bloodstream Infections (BSIs)
CRAB can cause bloodstream infections, especially in patients with indwelling vascular catheters, immunosuppression, or extensive burns. These infections are associated with septicemia, organ failure, and high mortality rates.
Wound and Surgical Site Infections
CRAB frequently infects post-surgical wounds, burn injuries, and traumatic wounds. These infections can lead to delayed healing, abscess formation, and systemic spread if not promptly managed.
Urinary Tract Infections (UTIs)
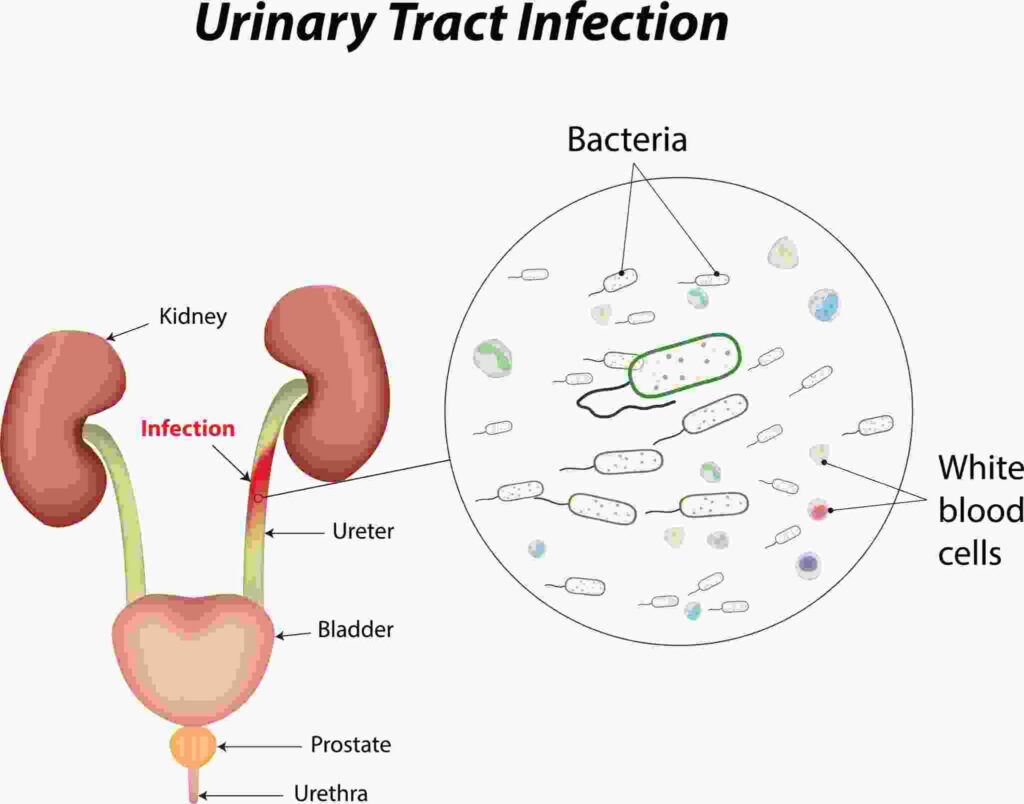
While less common, CRAB can cause complicated urinary tract infections, especially in catheterized patients. Symptoms may include dysuria, fever, and suprapubic pain, though presentations may be subtle in critically ill patients.
Laboratory Diagnosis of Carbapenem-Resistant Acinetobacter baumannii (CRAB)
Rapid and accurate laboratory diagnosis is essential for the management and control of CRAB infections. Several techniques are employed to identify the organism and determine its antibiotic susceptibility.
Culture and Identification
Clinical specimens from suspected infection sites are cultured on selective media such as MacConkey agar or blood agar. A. baumannii typically forms small, smooth, non-lactose fermenting colonies. Identification is confirmed using biochemical tests, automated systems (like VITEK), or mass spectrometry techniques like MALDI-TOF.
Antimicrobial Susceptibility Testing (AST)
Once identified, the bacterium’s susceptibility to various antibiotics is determined through disk diffusion, broth microdilution, or automated AST systems. Resistance to carbapenems is inferred from elevated MIC values for imipenem and meropenem.
Molecular Methods
Polymerase Chain Reaction (PCR) and DNA sequencing are employed to detect specific resistance genes, such as blaOXA-23, blaOXA-58, and blaNDM. These techniques offer rapid, sensitive, and specific identification of carbapenemase-producing strains.
Treatment Options for Carbapenem-Resistant Acinetobacter baumannii (CRAB) Infections
Managing CRAB infections is challenging due to the organism’s extensive drug resistance. Nonetheless, several therapeutic strategies are employed, often involving combination regimens to maximize efficacy.
Polymyxins
Polymyxins, particularly colistin and polymyxin B, are considered last-resort antibiotics for CRAB infections. While effective, they are associated with nephrotoxicity and neurotoxicity, necessitating careful monitoring.
Tigecycline
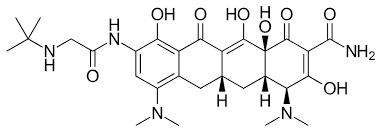
Tigecycline, a derivative of the tetracycline class, has demonstrated in vitro activity against CRAB, especially for intra-abdominal and soft tissue infections. However, its low serum concentrations limit its use in bloodstream infections.
Sulbactam-Based Combinations
Sulbactam possesses intrinsic activity against A. baumannii and is often combined with other β-lactams like ampicillin or cefoperazone to enhance therapeutic outcomes.
Novel Antibiotics
Cefiderocol, a siderophore cephalosporin, represents a promising new treatment option with potent activity against carbapenem-resistant gram-negative bacteria, including CRAB. Clinical trials are ongoing to validate its role in therapy.
Infection Control and Prevention
Effective infection control is pivotal in curbing CRAB transmission in healthcare settings. Strategies involve a combination of patient management protocols and environmental decontamination measures.
Hand Hygiene
Strict adherence to hand hygiene protocols using alcohol-based hand rubs or soap and water is the most effective strategy to prevent cross-transmission.
Environmental Cleaning
Regular cleaning and disinfection of hospital surfaces and equipment with appropriate agents can significantly reduce environmental contamination.
Patient Isolation
CRAB-infected or colonized patients should be placed in contact precautions, including the use of gowns and gloves by healthcare workers, to minimize the risk of transmission.
Surveillance and Antibiotic Stewardship
Active surveillance cultures and antibiotic stewardship programs help identify colonized patients early and optimize antimicrobial use, thereby reducing selective pressure and resistance emergence.
Conclusion
Carbapenem-Resistant Acinetobacter baumannii (CRAB) has become a significant healthcare concern due to its ability to cause severe, hard-to-treat infections and rapidly acquire resistance to multiple antibiotics, including carbapenems. Its resistance is primarily driven by carbapenemase production, efflux mechanisms, and porin loss, leaving limited treatment options such as polymyxins, tigecycline, and newer agents like cefiderocol. Carbapenem-Resistant Acinetobacter baumannii (CRAB) is associated with high morbidity and mortality, particularly in critically ill and immunocompromised patients. Controlling its spread requires strict infection prevention measures, active surveillance, and antimicrobial stewardship in healthcare settings. Additionally, early and accurate diagnosis using molecular methods and continuous investment in new drug development are essential to manage CRAB effectively and reduce its growing impact on global public health.
Frequently Asked Questions (FAQ)
Is CRE the same as CRAB?
No. CRE stands for Carbapenem-Resistant Enterobacteriaceae, a different group of bacteria resistant to carbapenems. CRAB refers specifically to Carbapenem-Resistant Acinetobacter baumannii, which belongs to a different bacterial family.
Is CRE the same as CRAB?
No. CRE stands for Carbapenem-Resistant Enterobacteriaceae, a different group of bacteria resistant to carbapenems. CRAB refers specifically to Carbapenem-Resistant Acinetobacter baumannii, which belongs to a different bacterial family.
What causes CRAB infection?
CRAB infections are caused by Carbapenem-Resistant Acinetobacter baumannii bacteria. They usually occur in hospitalized, critically ill, or immunocompromised patients, often through contaminated surfaces, medical devices, or hands of healthcare workers.
Related Contents
Candida tropicalis — Morphology, Habitat and Pathology
Candida albicans- Taxonomy , Morphology, Habitat and Pathology