Introduction
Candida parapsilosis is a type of yeast that naturally lives on human skin, mucous membranes, and in the gastrointestinal tract. While usually harmless in healthy individuals, it can cause serious infections, especially in people with weakened immune systems, premature babies, and those with medical devices like catheters or implants. Unlike its more notorious relative Candida albicans, C. parapsilosis has unique characteristics that influence how it spreads, infects, and resists treatment.
This overview covers its biology, risk factors, infections it causes, diagnosis, treatment, and prevention strategies.
Table of Contents
1. What is Candida parapsilosis?
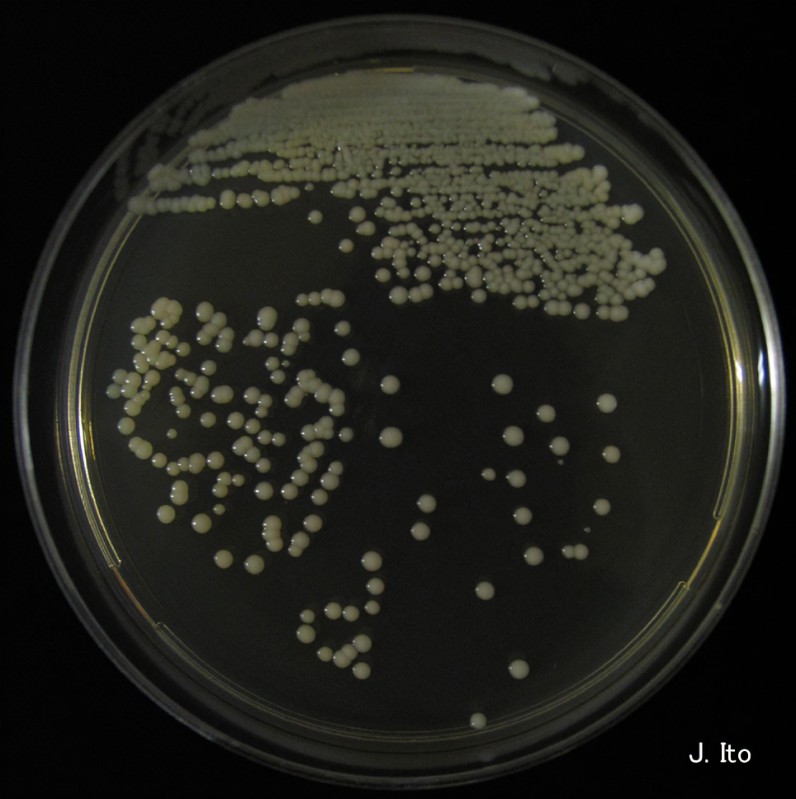
Candida parapsilosis is a fungus belonging to the Candida family. It is:
- Common in the environment – Found on skin, medical equipment, and healthcare surfaces.
- Opportunistic – Usually harmless but causes infections when the body’s defenses are low.
- A growing concern – Increasingly recognized as a cause of bloodstream infections (fungemia), particularly in hospitals.
2. How Does It Spread?
Unlike C. albicans, which often comes from the patient’s own body, C. parapsilosis frequently spreads through:
- Contaminated hands – Healthcare workers or patients touching infected surfaces.
- Medical devices – Catheters, IV lines, and surgical implants can harbor the yeast.
- Hospital surfaces – It survives on equipment, beds, and countertops.
This makes it a major cause of hospital-acquired infections.
3. Who is at Risk?
Certain groups are more vulnerable to C. parapsilosis infections:
- Newborns (especially premature babies) – Their underdeveloped immune systems struggle to fight fungal infections.
- ICU patients – Long hospital stays and invasive devices increase exposure.
- People with weakened immunity – Such as those with HIV/AIDS, cancer patients on chemotherapy, or organ transplant recipients on immunosuppressants.
- Surgical patients – Prosthetic implants (like heart valves or joints) can become infected.
- Diabetics – High blood sugar promotes fungal growth.
4. Types of Infections Caused
C. parapsilosis can lead to different infections, including:
A. Bloodstream Infections (Fungemia)
- Most common in hospitalized patients with central venous catheters.
- Symptoms: Fever, chills, low blood pressure (septic shock).
B. Endocarditis (Heart Valve Infection)
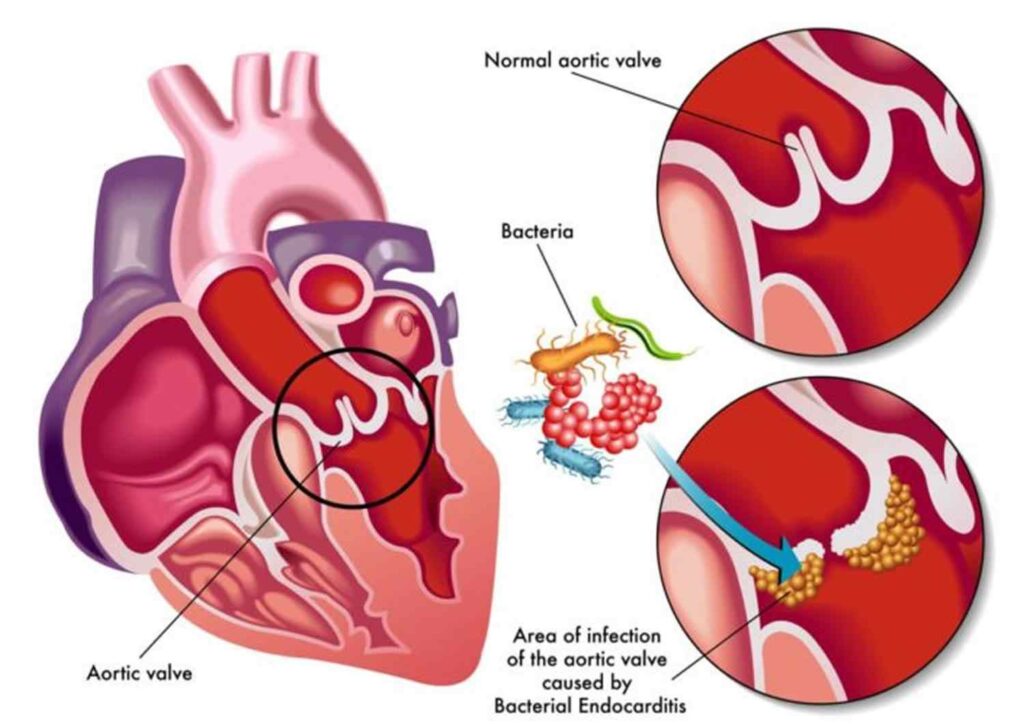
- Occurs after heart surgery or in IV drug users.
- Can damage heart valves, requiring surgery.
C. Wound and Tissue Infections
- Common in burn victims or after abdominal surgery.
- Delays healing and increases scarring risk.
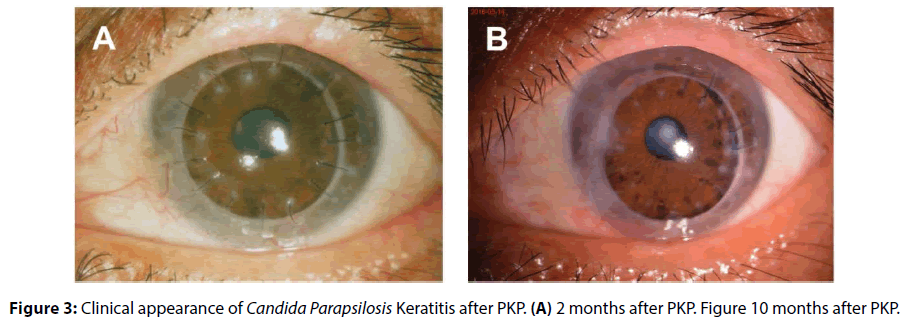
D. Eye Infections (Endophthalmitis)
- Can happen after eye surgery or trauma.
- May lead to vision loss if untreated.
E. Meningitis (Rare but Serious)
- Affects the brain and spinal cord.
- More common in premature babies or immunocompromised adults.
5. How is It Diagnosed?
Detecting C. parapsilosis involves:
- Blood cultures – The gold standard for bloodstream infections.
- Tissue biopsies – For wound or organ infections.
- Molecular tests (PCR) – Faster and more accurate than traditional cultures.
- Antifungal susceptibility testing – Helps determine the best treatment.
Since symptoms (fever, fatigue) mimic bacterial infections, doctors must specifically test for fungi.
6. Treatment Challenges
C. parapsilosis is often resistant to common antifungals like fluconazole. Treatment options include:
- Echinocandins (e.g., caspofungin) – First-line for bloodstream infections.
- Amphotericin B – Used for severe cases but has toxic side effects.
- Removing infected devices – Critical for catheter-related infections.
Treatment duration varies from weeks to months, depending on infection severity.
7. Prevention Strategies
Since C. parapsilosis thrives in hospitals, prevention focuses on:
- Strict hand hygiene – Alcohol-based sanitizers reduce transmission.
- Sterile catheter insertion – Proper techniques lower infection risks.
- Antifungal-coated medical devices – Emerging technology to prevent fungal growth.
- Early removal of unnecessary IV lines – Reduces exposure time.
8. Why is Candida parapsilosis Increasing?
Several factors contribute to its rise:
- Overuse of antibiotics – Kills bacteria, allowing fungi to grow unchecked.
- More invasive medical procedures – Implants and long-term catheters provide entry points.
- Better detection methods – More cases are now identified.
Conclusion
Candida parapsilosis is an emerging fungal pathogen, especially dangerous for hospitalized and immunocompromised patients. Unlike C. albicans, it spreads easily in healthcare settings through contaminated surfaces and medical devices. Early diagnosis, proper antifungal treatment, and strict infection control are crucial to managing its threat.
Research into better antifungals and preventive measures continues, as this yeast becomes a bigger challenge in modern medicine.
FREQUENTLY ASKED QUESTIONS
What is Candida parapsilosis?
Candida parapsilosis is a yeast-like fungus that can cause infections in humans. While it normally lives harmlessly on our skin and mucous membranes, it can lead to serious infections, especially in hospital settings or people with weakened immune systems.
How is it different from other Candida species?
Unlike Candida albicans which usually comes from a patient’s own body, C. parapsilosis:
1. Spreads more easily through contaminated surfaces and medical equipment
2. Forms stronger biofilms on plastic devices
3. Shows different patterns of antifungal resistance
4. Is more common in neonatal infections
What types of infections does it cause?
Common infections include:
1. Bloodstream infections (fungemia)
2. Heart valve infections (endocarditis)
3. Wound and surgical site infections
4. Peritonitis in dialysis patients
5. Eye infections (endophthalmitis)
6. Bone and joint infections
Related Articles