The CAMP test is a simple, yet very important diagnostic test used in microbiology. It is commonly performed in labs to identify specific types of bacteria, especially a type known as Group B Streptococcus (Streptococcus agalactiae). This test is widely used because it is easy to perform, does not require expensive equipment, and gives reliable results when done properly.
Let’s explore everything about the CAMP test in a step-by-step and clear way.
Table of Contents
1. What is the CAMP Test?
The CAMP test is a biochemical test used to identify Streptococcus agalactiae, also known as Group B Streptococcus (GBS).
The name CAMP comes from the initials of the scientists Christie, Atkins, and Munch-Petersen, who first described the test in 1944. They discovered that a substance produced by Streptococcus agalactiae enhances the activity of an enzyme called beta-hemolysin, produced by Staphylococcus aureus.
2. Principle of the CAMP Test
The principle of the CAMP test is based on the interaction between:
- CAMP factor: A protein produced by Streptococcus agalactiae
- Beta-hemolysin: An enzyme secreted by Staphylococcus aureus
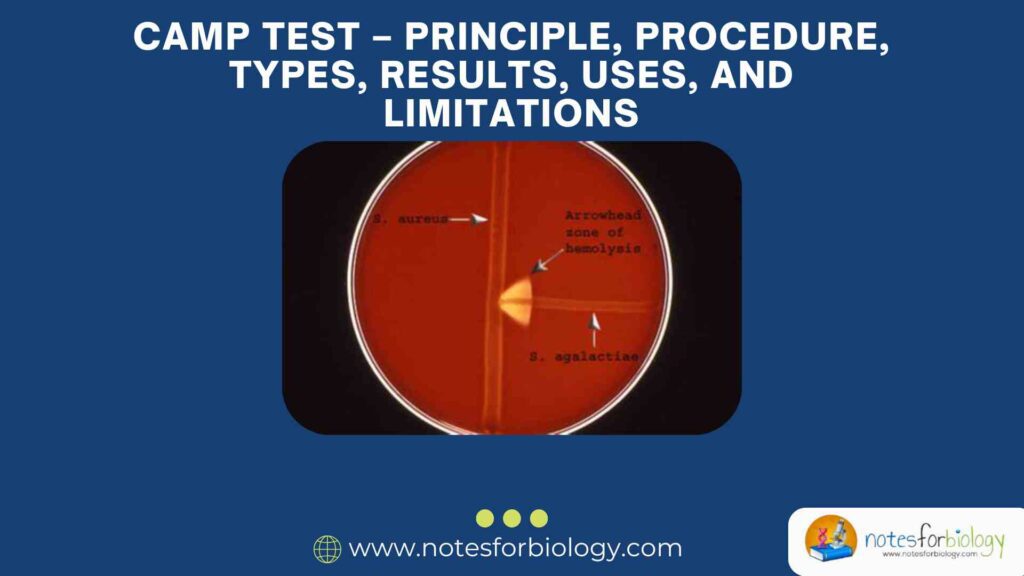
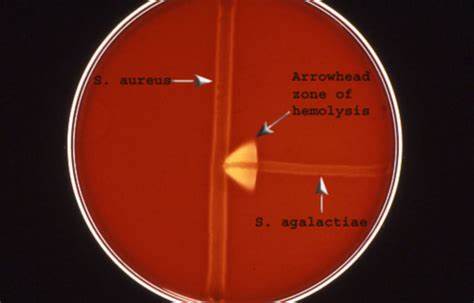
When both bacteria are grown near each other on a blood agar plate, the CAMP factor from S. agalactiae enhances the hemolytic activity (breaking down of red blood cells) of the beta-hemolysin from S. aureus. This results in an arrowhead-shaped zone of enhanced hemolysis at the junction where the two organisms meet.
This distinct zone of enhanced hemolysis is a positive CAMP test, which confirms the presence of Streptococcus agalactiae.
3. Materials Required
To perform the CAMP test, the following materials are needed:
- Blood agar plate (usually sheep blood)
- Pure culture of Staphylococcus aureus (beta-hemolysin-producing strain)
- Suspected culture of Streptococcus species
- Inoculating loop or swab
- Incubator (35–37°C)
- Sterile conditions (for safety and accuracy)
4. Procedure of the CAMP Test
Here is a step-by-step guide to how the CAMP test is performed:
Step 1: Label the blood agar plate
- Mark the plate to show where you will place Staphylococcus aureus and the test organism (suspected Streptococcus).
Step 2: Inoculate Staphylococcus aureus
- Using a sterile loop or swab, streak a straight line of S. aureus across the center of the blood agar plate (usually horizontally).
- Do not go all the way to the edge.
Step 3: Inoculate the test organism
- Take the suspected Streptococcus culture and streak a line perpendicular to the S. aureus line.
- Make sure the two streaks come close (1–2 mm apart) but do not touch.
Step 4: Incubate the plate
- Incubate the plate at 35–37°C for 18–24 hours in an aerobic environment.
5. Observing the Results
After incubation, observe the plate carefully.
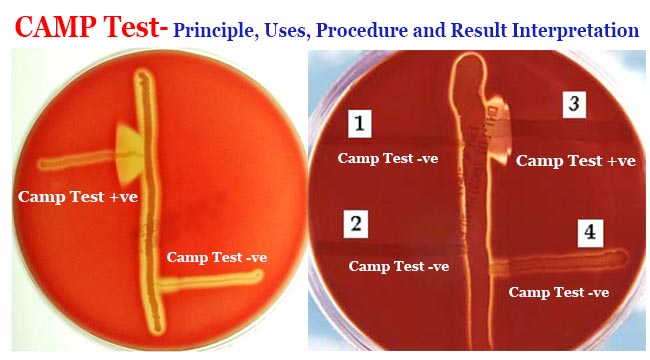
Positive CAMP Test Result:
- A clear, arrowhead-shaped zone of hemolysis (clear area) will appear at the point where the test organism comes close to the S. aureus line.
- This enhanced hemolysis is due to the interaction between CAMP factor and beta-hemolysin.
🡺 Positive Result = Group B Streptococcus (S. agalactiae)
Negative CAMP Test Result:
- No arrowhead-shaped hemolysis is seen.
- The hemolysis from S. aureus remains unchanged.
🡺 Negative Result = Not S. agalactiae (could be other Streptococcus species)
6. Types of CAMP Test
There are a few different variations of the CAMP test depending on the technique used. The most common types are:
A. Classic Streak Method (Standard CAMP Test)
This is the method described above, where the S. aureus and the test organism are streaked on a blood agar plate.
B. Reverse CAMP Test
- Used especially for identifying Clostridium perfringens.
- In this test, Clostridium perfringens (which produces alpha toxin) is streaked on the agar.
- A Group B Streptococcus strain is streaked perpendicularly to it.
- The interaction between the CAMP factor and alpha toxin causes inhibition of hemolysis, forming a narrow zone.
C. Microtiter Plate CAMP Test
- Uses liquid media in wells of a plate.
- Less common, usually for research.
- Can be used for testing multiple samples quickly.
7. Uses of the CAMP Test
The CAMP test has several important uses in medical microbiology:
1. Identification of Group B Streptococcus (S. agalactiae)
- This is the main use of the CAMP test.
- Especially important in pregnant women since Group B Streptococcus can infect newborns during delivery.
2. Differentiation from Other Streptococci
- Helps to distinguish S. agalactiae from other Streptococcus species such as:
- S. pyogenes (Group A) → CAMP negative
- S. pneumoniae → CAMP negative
3. Diagnostic Support in Neonatal Infections
- Group B Streptococcus can cause meningitis, pneumonia, and sepsis in newborns.
- Early identification is crucial for treatment.
4. Reverse CAMP Test for Clostridium perfringens
- Helps identify this bacterium which causes gas gangrene and food poisoning.
8. Advantages of the CAMP Test
- Simple to perform
- Inexpensive
- Gives quick and reliable results
- Widely accepted and recognized
- Requires basic lab materials
9. Limitations of the CAMP Test
Like all tests, the CAMP test has some limitations:
1. Not 100% Specific
- Rarely, other bacteria might show weak CAMP-like reactions.
- Requires confirmatory tests for absolute identification.
2. Depends on Beta-Hemolysin Production
- The test will not work if the Staphylococcus aureus strain does not produce enough beta-hemolysin.
3. Interpretation Can Be Subjective
- Reading the arrowhead zone of hemolysis requires experience.
- Very weak reactions might be misread.
4. False Negatives Can Occur
- If the bacteria are not fresh or viable, CAMP factor may not be produced.
- Incorrect technique (e.g., streaks too far apart or touching) can also give wrong results.
10. Safety Considerations
When performing the CAMP test, it’s important to follow safety rules:
- Always work in a sterile environment.
- Wear gloves and lab coats.
- Dispose of all biological waste properly.
- Handle Staphylococcus aureus and Streptococcus cultures carefully, as they can be potentially pathogenic.
11. Confirmatory Tests After CAMP
If a CAMP test is positive, further testing can be done for confirmation:
- Bile Esculin Test
- Hippurate hydrolysis test
- Latex agglutination test for Group B antigen
- PCR (Polymerase Chain Reaction) for genetic confirmation
- MALDI-TOF MS in advanced labs
12. Real-life Application: Pregnancy and Group B Strep
In many hospitals, pregnant women are screened for Group B Streptococcus around 35–37 weeks of pregnancy.

- A positive test means the mother carries the bacteria.
- Antibiotics are given during labor to prevent transmission to the baby.
- This reduces the risk of neonatal sepsis and meningitis.
CAMP test is often one of the preliminary tests used in this process, especially in settings without advanced molecular tools.
Conclusion
The CAMP test is a valuable and reliable test in the field of microbiology. Though it may look simple, it plays a crucial role in diagnosing bacterial infections, especially those caused by Streptococcus agalactiae.
By understanding its principle, procedure, types, and limitations, we can use it more effectively and responsibly. Whether you are a student, a lab worker, or a clinician, knowing how this test works helps you appreciate the science behind accurate bacterial diagnosis.
FREQUENTLY ASKED QUESTIONS
What is the CAMP test?
The CAMP test is a microbiological test used to identify Streptococcus agalactiae (Group B Streptococcus). It detects the presence of a special protein (CAMP factor) that enhances the hemolysis caused by Staphylococcus aureus.
Why is it called the “CAMP” test?
It is named after the scientists Christie, Atkins, and Munch-Petersen, who discovered the phenomenon in 1944.
What media is used for the CAMP test?
A sheep blood agar plate is commonly used, as it supports the growth of both bacteria and clearly shows hemolysis.
Related Articles