Detecting pathogenic bacteria in the bloodstream is critically important because these infections can rapidly progress to life-threatening conditions. Bloodstream infections (BSIs) represent a serious medical challenge worldwide due to their high morbidity and mortality rates. Understanding the bacteria responsible, their mechanisms of entry, and appropriate management strategies is essential to improving patient outcomes.
BSIs often lead to systemic inflammatory responses known as sepsis, which requires urgent diagnosis and treatment to prevent organ failure and death. This article provides a comprehensive overview of BSIs, the common bacterial pathogens involved, diagnostic approaches, and current treatment and prevention strategies.
Summary of Bloodstream Infections (BSIs)
- Bloodstream infections (BSIs) occur when pathogenic microorganisms such as bacteria or fungi enter the bloodstream, potentially causing severe systemic illness including sepsis.
- BSIs can arise from various sources including infected medical devices, wounds, or secondary to infections elsewhere in the body, and are more common in hospitalized or immunocompromised patients.
- Early diagnosis through blood cultures and prompt, targeted antimicrobial therapy are crucial to reduce morbidity and mortality associated with BSIs.
Table of Contents
What Are Bloodstream Infections (BSIs)?
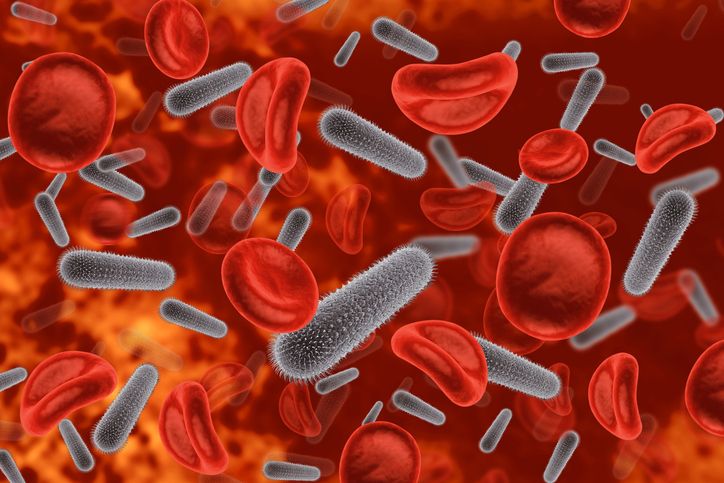
Bloodstream infections refer to the presence of pathogenic microorganisms, predominantly bacteria, in the blood, which can result in systemic illness. These infections may originate from localized sites or directly enter the bloodstream through medical interventions.
BSIs are broadly classified into primary infections, where the blood is the initial site, and secondary infections, where bacteria spread from another infected focus. Early identification of these infections is vital to prevent complications.
Definition and Classification of Bloodstream Infections (BSIs)
BSIs occur when bacteria or other pathogens enter the bloodstream and multiply, potentially causing systemic infection. They are generally classified into two categories: primary bloodstream infections, originating directly in the blood (e.g., catheter-related infections), and secondary bloodstream infections, arising from other infected tissues like pneumonia or urinary tract infections.
This classification aids clinicians in tracing the infection source and tailoring treatment effectively.
How Pathogenic Bacteria Enter the Bloodstream
Pathogenic bacteria can enter the bloodstream through several routes, including breaches in the skin barrier, invasive medical devices such as intravenous catheters, surgical procedures, or from localized infections that spread hematogenously.
The disruption of natural protective barriers and immune suppression are key factors facilitating bacterial entry and bloodstream invasion.
Risk Factors for Blood Infections
Certain populations are at higher risk for bloodstream infections. These include hospitalized patients with indwelling devices, immunocompromised individuals (such as cancer patients or those with HIV), the elderly, neonates, and patients undergoing invasive procedures.
Underlying chronic diseases, poor hygiene, and prolonged antibiotic use also increase susceptibility to BSIs.
Why Are Blood Infections Dangerous?
Blood infections are dangerous due to the bloodstream’s role in transporting pathogens and toxins throughout the body, allowing rapid dissemination and systemic inflammatory responses.
If untreated, BSIs can progress to septicemia and severe sepsis, conditions associated with multi-organ dysfunction and high mortality rates worldwide. Prompt recognition and intervention are critical.
Rapid Spread of Toxins and Pathogens
Once bacteria enter the bloodstream, they release endotoxins and exotoxins that trigger a widespread inflammatory cascade. This can result in systemic vasodilation, capillary leak, and tissue hypoperfusion, leading to shock.
The rapid systemic spread of pathogens can overwhelm the immune system, causing significant damage to organs.
Potential for Septicemia and Sepsis
Septicemia describes the presence of viable bacteria in the blood that causes symptoms of infection. Sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection, is a major consequence of untreated or poorly managed BSIs.
Early signs of sepsis include fever, chills, rapid heartbeat, and confusion, requiring urgent medical care.
Mortality Rates and Global Statistics
BSIs and sepsis contribute to millions of deaths globally each year, especially in low- and middle-income countries. Mortality rates vary depending on the pathogen, patient comorbidities, and healthcare quality but can exceed 30% in severe sepsis cases.
Global efforts are underway to improve early diagnosis and treatment to reduce this burden.
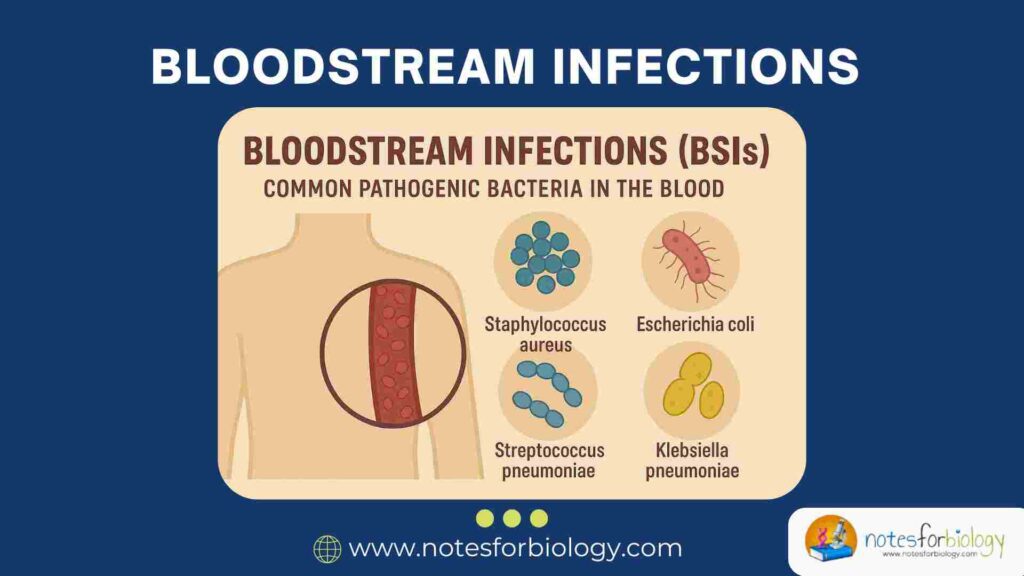
Common Pathogenic Bacteria Found in Blood
Several bacterial species are commonly isolated from blood cultures in BSIs. These bacteria vary in virulence, resistance patterns, and the infections they cause. Understanding their characteristics helps guide clinical management.
Staphylococcus aureus
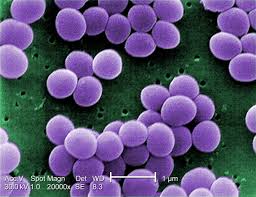
Staphylococcus aureus is a leading cause of both community-acquired and hospital-acquired bloodstream infections.
Characteristics
It is a Gram-positive coccus capable of producing a variety of virulence factors including toxins and enzymes that facilitate tissue invasion and immune evasion. Methicillin-resistant Staphylococcus aureus (MRSA) strains are especially concerning due to antibiotic resistance.
Common Infections
S. aureus BSIs often originate from skin infections, pneumonia, or infected medical devices such as catheters and prosthetic implants. These infections can lead to complications like endocarditis and osteomyelitis.
Treatment Options
Treatment depends on antibiotic susceptibility. Methicillin-sensitive strains are treated with beta-lactams, whereas MRSA infections require agents such as vancomycin or linezolid. Prompt removal of infected devices is also important.
Escherichia coli (E. coli)
Escherichia coli is a frequent cause of bloodstream infections, especially secondary to urinary tract infections and intra-abdominal infections.
Strains Involved in Blood Infections
Certain virulent strains of E. coli possess adhesins, toxins, and capsules that enhance their ability to invade the bloodstream. These strains are commonly involved in sepsis originating from urinary or gastrointestinal sources.
Clinical Symptoms
Patients with E. coli BSIs typically present with fever, chills, hypotension, and signs related to the primary infection site. The infection can progress rapidly without appropriate treatment.
Treatment Guidelines
Empirical therapy often includes broad-spectrum antibiotics such as third-generation cephalosporins or carbapenems, adjusted based on susceptibility results. Resistance patterns, including ESBL production, complicate therapy.
Streptococcus pneumoniae
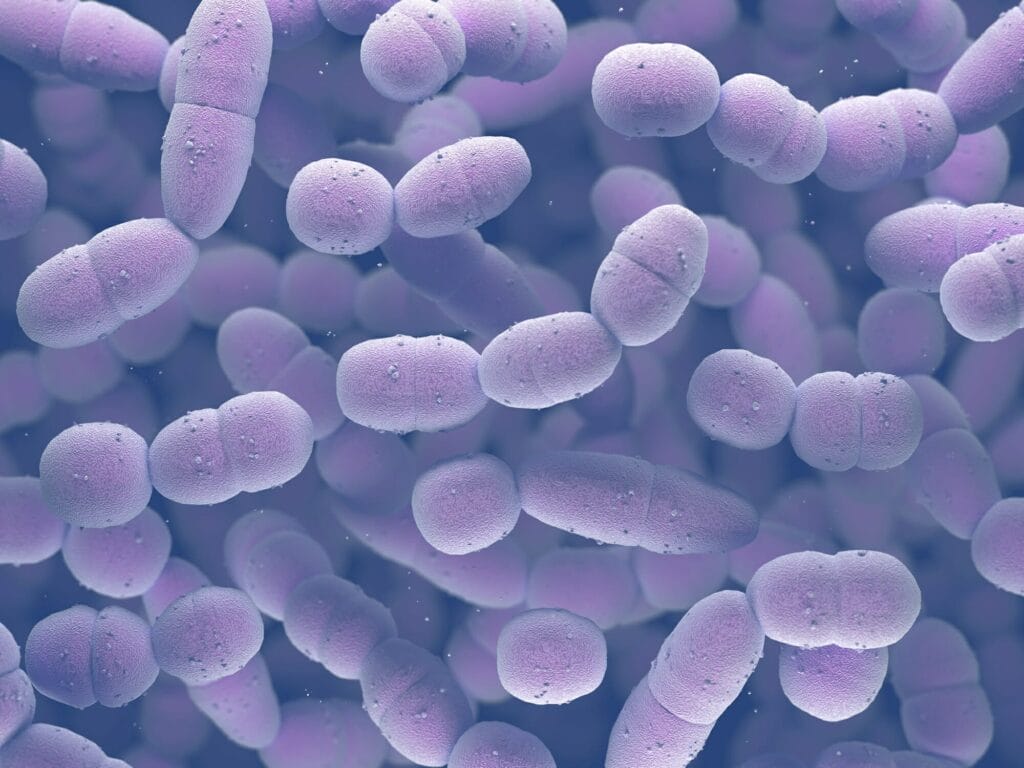
A major pathogen causing both pneumonia and invasive bloodstream infections, particularly in children and the elderly.
Involvement in Pneumonia and Bloodstream Infections
S. pneumoniae frequently causes bacteremia secondary to pneumonia or meningitis. It is characterized by a polysaccharide capsule that aids in immune evasion.
Diagnostic Features
Blood cultures and antigen detection tests assist in confirming infection. Pneumococcal infections often present with respiratory distress and systemic inflammatory signs.
Antibiotic Sensitivity
While many strains remain sensitive to penicillin and cephalosporins, resistance is increasing, necessitating susceptibility testing and sometimes combination therapy.
Klebsiella pneumoniae
An opportunistic pathogen and important cause of hospital-acquired BSIs.
Multidrug-Resistant Strains
Klebsiella species frequently harbor resistance genes, including ESBLs and carbapenemases, making infections difficult to treat.
Hospital-Acquired Infections
They commonly cause infections related to invasive devices, surgery, or immunocompromised states in healthcare settings.
Treatment Approaches
Treatment requires antibiotic susceptibility guidance, often involving carbapenems, polymyxins, or newer beta-lactam/beta-lactamase inhibitor combinations.
Pseudomonas aeruginosa
A Gram-negative opportunistic pathogen causing severe infections in hospitalized or immunocompromised patients.
Opportunistic Pathogen Profile
Pseudomonas thrives in moist hospital environments and is notorious for forming biofilms on medical equipment.
Common Clinical Settings
It causes bloodstream infections particularly in patients with burns, neutropenia, or indwelling catheters.
Antibiotic Resistance Issues
Multidrug resistance is common, requiring combination therapies and susceptibility-guided treatments.
Enterococcus faecalis and Enterococcus faecium
Gram-positive cocci commonly involved in nosocomial bloodstream infections.
Role in Nosocomial Infections
They are significant causes of catheter-associated BSIs and infective endocarditis, often resistant to multiple antibiotics.
Clinical Management
Treatment can be challenging due to resistance to cephalosporins and aminoglycosides; agents like vancomycin or linezolid are used, sometimes in combination.
Neisseria meningitidis
A fast-progressing pathogen linked to meningococcemia and bloodstream infections.
Link to Meningococcemia
N. meningitidis rapidly invades the bloodstream, causing severe sepsis with characteristic rash and high fatality rates if untreated.
Rapid Progression Symptoms
Symptoms include sudden fever, chills, hypotension, and petechial rash, requiring urgent hospitalization.
Vaccine and Antibiotic Therapies
Vaccination has significantly reduced incidence, and treatment involves prompt administration of penicillin or third-generation cephalosporins.
Diagnostic Methods for Blood Infections
Early and accurate diagnosis of BSIs is critical for effective treatment. Multiple laboratory techniques are employed for detection.
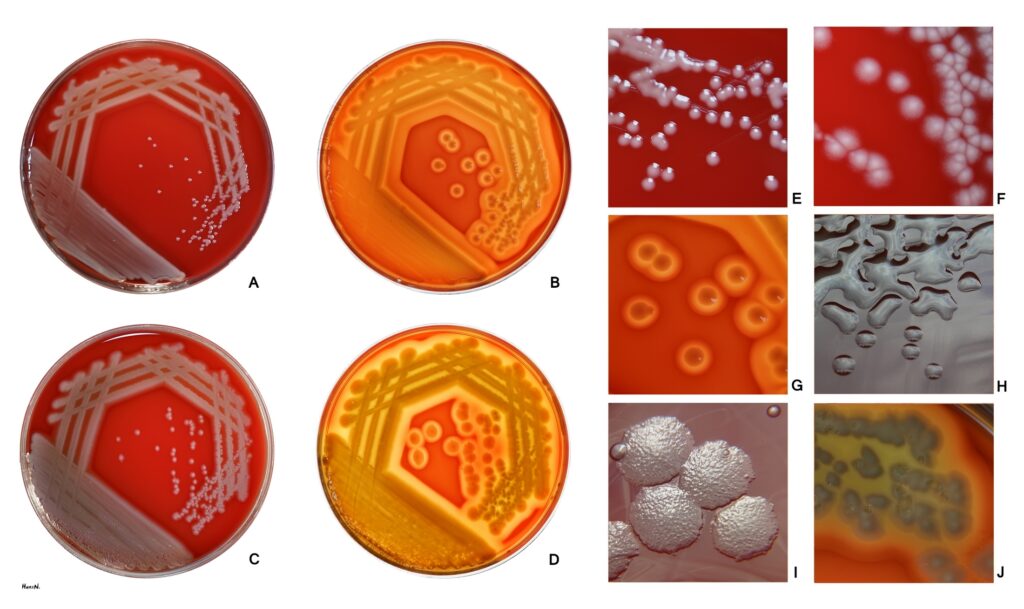
Blood Culture Techniques
Blood culture remains the gold standard for diagnosing BSIs. It involves culturing patient blood samples to identify causative organisms and determine antibiotic susceptibility.
PCR and Molecular Diagnostics
Molecular methods like PCR offer rapid detection of bacterial DNA, even before cultures become positive. They improve diagnostic speed and can detect difficult-to-culture organisms.
Procalcitonin and Biomarker Testing
Procalcitonin is a biomarker elevated in bacterial infections and sepsis. It aids in distinguishing bacterial from viral infections and guiding antibiotic therapy.
Treatment Strategies
Timely administration of appropriate antibiotics, supportive care, and infection source control are fundamental in managing BSIs.
Empiric Antibiotic Therapy
Empirical broad-spectrum antibiotics are initiated promptly upon suspicion of BSI, tailored later based on culture results to optimize efficacy and minimize resistance.
Targeted Antimicrobial Stewardship
Stewardship programs promote the judicious use of antibiotics, ensuring appropriate choice, dose, and duration to improve outcomes and reduce resistance.
Supportive Care in Sepsis Management
Management of sepsis includes fluid resuscitation, vasopressors, respiratory support, and monitoring organ function to reduce mortality.
Prevention of Bloodstream Infections
Preventive measures focus on reducing hospital-acquired infections and protecting vulnerable patients.
Hospital Infection Control Protocols
Strict adherence to sterile techniques, hand hygiene, and environmental cleaning significantly lowers BSI rates.
Importance of Hand Hygiene and Sterile Techniques
Hand washing and use of sterile gloves during invasive procedures are essential to prevent pathogen transmission.
Prophylactic Antibiotics in High-Risk Patients
Prophylaxis may be considered in selected patients undergoing high-risk procedures or with compromised immunity to prevent BSIs.
Emerging Threats: Multidrug-Resistant Bacteria in Blood
Antimicrobial resistance complicates the management of BSIs globally.
MRSA (Methicillin-Resistant Staphylococcus aureus)
MRSA is a major challenge in treating staphylococcal BSIs due to resistance to many antibiotics, necessitating the use of alternatives like vancomycin.
ESBL-Producing Enterobacteriaceae
Extended-spectrum beta-lactamase (ESBL) producing bacteria such as E. coli and Klebsiella resist many beta-lactams, limiting treatment options.
Carbapenem-Resistant Bacteria
Carbapenem-resistant organisms, including Klebsiella and Pseudomonas species, are increasingly reported, posing significant treatment difficulties.
Conclusion
Bloodstream infections caused by pathogenic bacteria represent a critical threat to global health due to their rapid progression and high mortality. The spectrum of bacterial pathogens includes common organisms like Staphylococcus aureus and E. coli, as well as multidrug-resistant strains complicating treatment.
Early diagnosis, prompt administration of targeted antibiotics, and rigorous infection prevention strategies are essential to improving patient outcomes. Continuous surveillance and antimicrobial stewardship remain vital in combating emerging resistant pathogens in blood infections.
Frequently Asked Questions (FAQ)
What are the first signs of a blood infection?
Fever, chills, rapid heartbeat, low blood pressure, and confusion are early warning signs.
How is a blood infection diagnosed?
Diagnosis is primarily through blood cultures, supported by molecular tests and biomarkers like procalcitonin.
Which bacteria are most dangerous in blood infections?
Staphylococcus aureus (including MRSA), E. coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa are among the most dangerous pathogens.
Related Contents
Common Bacteria Causing UTI (Urinary Tract Infection)
Columbia Agar with 5% Sheep Blood- Composition, Principle, Preparation, Results, Uses