Introduction
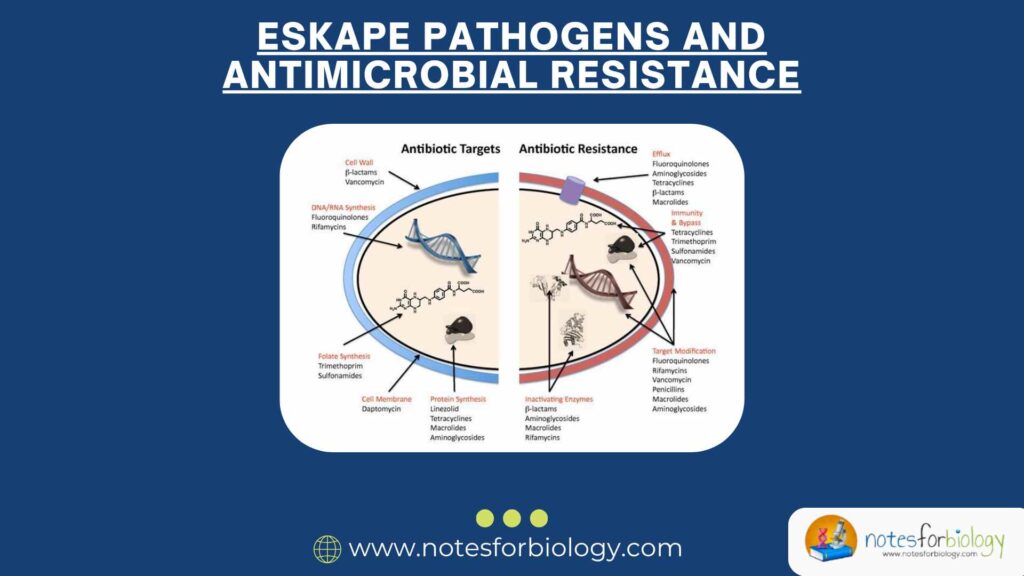
Antibiotics are powerful and life-saving medicines that have been used for many years to fight infections caused by bacteria. These medicines work by killing bacteria or stopping their growth so that our bodies can recover. Since the discovery of penicillin, antibiotics have been a major tool in modern medicine. They have saved millions of lives and allowed doctors to treat infections that used to be deadly. However, bacteria are living organisms that can change and adapt. Over time, they have developed special abilities to survive even when antibiotics are used against them. This problem is known as antimicrobial resistance (AMR).
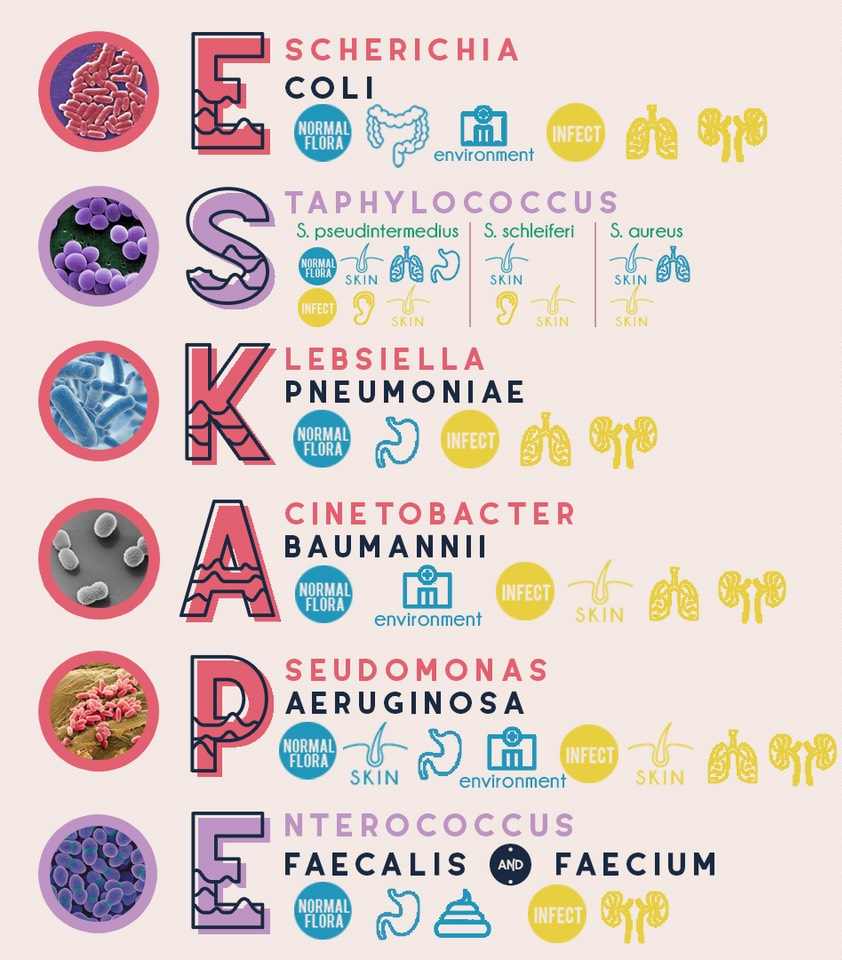
Antimicrobial resistance means that antibiotics and similar drugs become less effective, making infections harder to treat. Among all the different kinds of bacteria, a specific group known as ESKAPE pathogens has become especially dangerous. These bacteria are called ESKAPE pathogens because the first letters of their names spell the word “ESKAPE,” and they are known for their ability to “escape” the effects of antibiotics.
- E – Enterococcus faecium
- S – Staphylococcus aureus
- K – Klebsiella pneumoniae
- A – Acinetobacter baumannii
- P – Pseudomonas aeruginosa
- E – Enterobacter species
These six bacteria are responsible for many serious infections, especially in hospitals. They have become resistant to many antibiotics, making them difficult to treat. In this guide, we will explore what these bacteria are, how they cause infections, why they are resistant to antibiotics, and what we can do to stop them from spreading.
Table of Contents
What Are ESKAPE Pathogens?
ESKAPE pathogens are a group of bacteria that have become well-known for causing infections in hospitals and healthcare settings. They are particularly dangerous because they can resist the effects of many antibiotics that are normally used to treat infections. This makes them a major concern for doctors, nurses, and scientists around the world.
These bacteria are commonly found in places like hospitals where people may already be sick or have weak immune systems. They can cause serious infections in patients who have wounds, breathing tubes, catheters, or are recovering from surgery. Because these bacteria can survive in tough environments and are difficult to kill, they often lead to longer hospital stays, higher medical costs, and sometimes even death.
Let’s take a closer look at each of the ESKAPE pathogens to understand how they work and why they are so dangerous.
Enterococcus faecium
Characteristics
- It is a Gram-positive bacterium, which means it has a thick outer cell wall.
- It is normally found in the human intestines and doesn’t cause problems in healthy people.
- However, it can survive for a long time in hospital settings and infect sick patients.
Infections Caused
- Urinary tract infections (UTIs): These are infections that affect the bladder and urinary system.
- Bloodstream infections: When the bacteria enter the blood, they can spread throughout the body.
- Wound infections: Especially in patients who have surgery or open wounds.
Resistance
This bacterium has developed resistance to many antibiotics, especially vancomycin, a drug that is often used when other antibiotics fail. When Enterococcus faecium becomes resistant to vancomycin, it is called vancomycin-resistant enterococci (VRE). Treating infections caused by VRE is very difficult and may require strong or multiple antibiotics.
Control Measures
- Hospitals should make sure all healthcare workers wash their hands properly.
- Patients who are infected should be placed in separate rooms to avoid spreading the bacteria.
- Doctors should be careful when prescribing antibiotics to avoid making resistance worse.
Staphylococcus aureus
Characteristics
- It is a Gram-positive bacterium with a round shape (coccus).
- It lives on the skin and in the nose of many people without causing harm.
- It can cause infections when it enters the body through cuts or medical procedures.
Infections Caused
- Skin infections: Such as boils, abscesses, and pimples.
- Pneumonia: A lung infection that can be serious in sick or elderly patients.
- Bloodstream infections: Known as sepsis, can be life-threatening.
- Surgical wound infections: Infections that occur after surgery.
Resistance
Some forms of this bacterium have become resistant to methicillin, an antibiotic once commonly used to treat it. These strains are called methicillin-resistant Staphylococcus aureus (MRSA). MRSA infections are much harder to treat and require different antibiotics.
Control Measures
- Hospitals must take strict precautions, like using gloves and gowns.
- Patients can be tested to see if they carry MRSA and treated before surgery.
- Doctors should use strong antibiotics only when needed to prevent further resistance.
Klebsiella pneumoniae
Characteristics
- A Gram-negative rod-shaped bacterium that has a thick outer capsule.
- Normally found in the human digestive system, where it does not usually cause harm.
- In hospitals, it can spread easily and infect patients.
Infections Caused
- Pneumonia: Particularly dangerous in people who are on ventilators.
- Urinary tract infections: Especially in patients with catheters.
- Bloodstream infections: Can lead to shock and organ failure.
- Meningitis: A serious infection of the brain and spinal cord.
Resistance
This bacterium can produce enzymes called carbapenemases that break down even powerful antibiotics like carbapenems. These resistant strains are called carbapenem-resistant Klebsiella pneumoniae (CRKP) and are very dangerous.
Control Measures
- Infections should be detected early using lab tests.
- Infected patients must be treated in isolated areas.
- Proper use of antibiotics and cleanliness are crucial to prevent spread.
Acinetobacter baumannii
Characteristics
- A Gram-negative bacterium found in soil and water.
- Known for surviving on surfaces like bed rails, doorknobs, and equipment.
- Mostly affects patients in intensive care units.
Infections Caused
- Pneumonia: Often in patients using ventilators.
- Bloodstream infections: Can spread quickly and become severe.
- Wound infections: Common in soldiers and trauma patients.
- Urinary tract infections: Usually associated with catheters.
Resistance
This bacterium can resist many antibiotics. It often survives cleaning and forms a protective biofilm that makes it harder to remove. Some strains are resistant to nearly all available drugs.
Control Measures
- Hospitals must disinfect surfaces regularly and thoroughly.
- Limiting the use of invasive devices can reduce infection risk.
- Antibiotics should be prescribed with care to avoid promoting resistance.
Pseudomonas aeruginosa
Characteristics
- A Gram-negative rod-shaped bacterium that thrives in moist places.
- Found in water, soil, and hospital environments.
- Known for its natural resistance to many antibiotics.
Infections Caused
- Lung infections: Especially dangerous for patients with cystic fibrosis.
- Urinary tract infections: More common with catheter use.
- Bloodstream infections: Can cause rapid health decline.
- Wound and burn infections: Hard to treat and slow to heal.
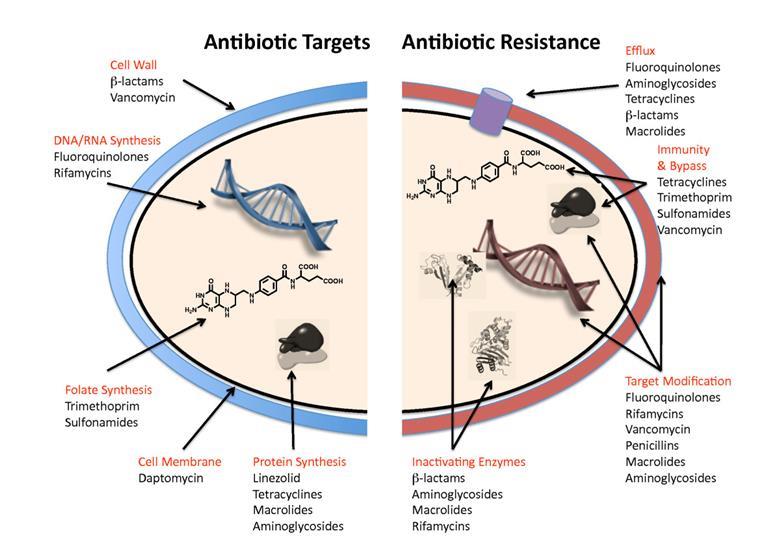
Resistance
Pseudomonas uses various methods to avoid antibiotics. It can pump out drugs using proteins in its cell membrane and produce enzymes that break down medications. It also forms biofilms, which act like a shield.
Control Measures
- Hospital equipment must be cleaned and sterilized.
- Early treatment with appropriate antibiotics is necessary.
- Monitoring resistance patterns helps choose the right drugs.
Enterobacter Species
Characteristics
- A group of Gram-negative bacteria normally living in the intestines.
- Can become harmful in hospitals or when they enter the bloodstream.
Infections Caused
- Bloodstream infections: Can cause fever and inflammation.
- Urinary tract infections: Especially in elderly and hospitalized patients.
- Lung infections: Can cause serious breathing problems.
Resistance
These bacteria often produce enzymes called beta-lactamases that destroy common antibiotics. They can quickly become resistant during treatment, making it hard to choose the right drug.
Control Measures
- Using the right antibiotic based on lab tests.
- Keeping a close watch on resistance changes.
- Practicing good hygiene and infection control.
Why Are ESKAPE Pathogens Important?
These six bacteria (ESKAPE Pathogens) are very important because they are leading causes of hospital-acquired infections. What makes them especially dangerous is their resistance to multiple antibiotics. When regular treatments stop working, infections last longer and become more severe. Patients may need stronger and more expensive drugs, and sometimes, even those don’t work.
These pathogens (ESKAPE Pathogens) can spread quickly in hospitals where patients are already sick. They survive on surfaces, can live in harsh conditions, and pass easily from one patient to another through contact. Because of all these reasons, ESKAPE pathogens are among the top threats in global healthcare.
Antimicrobial Resistance (AMR)
AMR is when bacteria and other microbes no longer respond to drugs that used to kill them. This happens because microbes can change and become stronger. AMR is not only a health problem; it is also a social and economic challenge. It increases treatment costs, causes longer hospital stays, and leads to higher death rates.
Causes of Antimicrobial Resistance
- Overuse of Antibiotics: Taking antibiotics for things like the common cold, which is caused by viruses, does not help and allows bacteria to build resistance.
- Incomplete Dosage: Stopping antibiotics early can let surviving bacteria become stronger and more dangerous.
- Poor Infection Control: Without proper hand washing or disinfection, resistant bacteria spread easily in hospitals.
- Antibiotic Use in Animals: Giving antibiotics to farm animals for growth, not just for illness, contributes to resistance.
- Global Travel: People traveling from one country to another can unknowingly carry resistant bacteria with them.
How Can We Fight AMR and ESKAPE Pathogens?
1. Proper Antibiotic Use
- Only take antibiotics when a doctor prescribes them.
- Never use old or leftover antibiotics.
- Always finish the full treatment, even if you feel better.
2. Infection Control in Hospitals
- Healthcare workers must wash hands and use gloves.
- Equipment and rooms must be cleaned regularly.
- Isolate patients with resistant infections when needed.
3. Surveillance and Monitoring
- Track and record resistance patterns.
- Share data with hospitals, labs, and governments.
4. Research and New Treatments
- Support research to find new antibiotics.
- Explore alternative methods like bacteriophages.
- Develop vaccines to prevent infections in the first place.
5. Education and Awareness
- Inform doctors, nurses, and the public about resistance.
- Promote responsible use of antibiotics at all levels.
Conclusion
The ESKAPE pathogens are a serious and growing threat to global health. These six types of ESKAPE Pathogens bacteria are difficult to kill because they have become resistant to many antibiotics. They cause dangerous infections, especially in hospitals, and can be life-threatening.
Antimicrobial resistance is a challenge we must all work to fight. Through responsible antibiotic use, better hygiene, smart research, and global cooperation, we can reduce the spread of resistance. Everyone—patients, healthcare workers, researchers, and governments—has a role to play in this battle.
Three Key Summary
- ESKAPE pathogens are a group of dangerous bacteria that are resistant to many antibiotics and often cause hospital infections.
- Antimicrobial resistance makes it harder and more expensive to treat infections, putting lives at risk.
- We can fight resistance of ESKAPE Pathogens by using antibiotics wisely, improving hygiene, and supporting research for new treatments.
FREQUENTLY ASKED QUESTIONS
What are ESKAPE pathogens?
They are six dangerous bacteria that resist antibiotics and cause serious hospital infections.
Why are they called ESKAPE pathogens?
Because their names begin with the letters E, S, K, A, P, and E, and they “escape” the effects of antibiotics.
What is antimicrobial resistance?
It is when bacteria and other microbes change so they are no longer killed by the drugs meant to treat them.
Related Articles