Bacteria display a remarkable diversity of shapes, with each morphological type offering insights into their physiology, pathogenesis, and clinical relevance. Among these, coccobacilli are a unique intermediate form between cocci (spherical) and bacilli (rod-shaped) bacteria.
Understanding coccobacilli is crucial in clinical microbiology and infectious disease management because several significant human pathogens fall within this category. This article will explain their definition, structure, classification, clinical significance, laboratory identification, diseases caused, and therapeutic approaches.
Table of Contents
Definition of Coccobacilli Bacteria
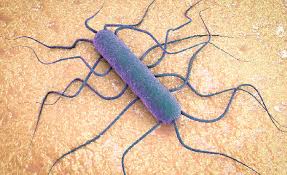
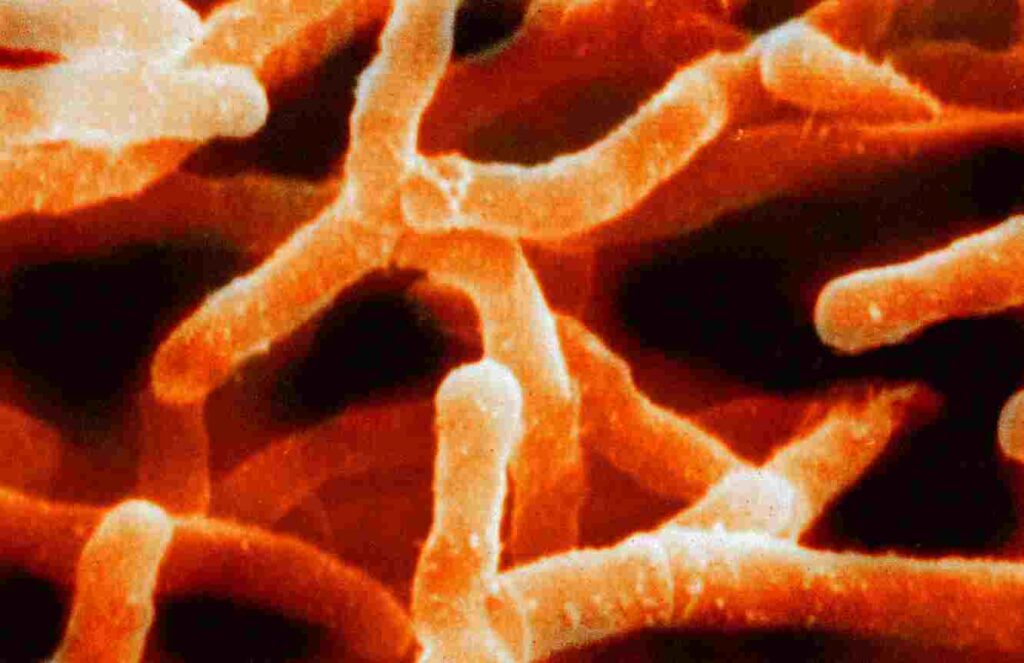
Coccobacilli are short, oval-shaped bacteria that possess features intermediate between cocci and bacilli. They appear either slightly elongated or oval under a microscope, making them difficult to classify without additional staining and laboratory techniques.
This morphology allows them to adapt to various environments and contributes to their role in multiple infectious diseases affecting humans and animals.
Importance in Clinical Microbiology and Infectious Diseases
Coccobacilli are medically important because many pathogenic species within this group are responsible for life-threatening conditions such as meningitis, whooping cough, listeriosis, and zoonotic infections like brucellosis and tularemia.
Correct identification and timely treatment of coccobacilli infections are essential, given their diverse antimicrobial resistance profiles and rapid progression in severe cases.
What are Coccobacilli?
Coccobacilli represent a morphological category of bacteria positioned between cocci and bacilli. Their physical structure influences their staining properties, growth patterns, and pathogenic potential.
Morphological Definition
Coccobacilli are defined by their short, plump, rod-like appearance, often resembling an elongated coccus or a shortened bacillus. This morphology can sometimes create diagnostic challenges under a microscope, especially in direct clinical specimens.
How They Differ from Cocci and Bacilli
Unlike cocci, which are spherical, and bacilli, which are cylindrical and elongated, coccobacilli exhibit an intermediate oval shape. While cocci cluster in groups or chains and bacilli form long rods, coccobacilli are typically seen singly or in pairs.
Their distinctive shape affects their motility, colony morphology, and virulence characteristics.
Gram-Positive vs. Gram-Negative Coccobacilli
Coccobacilli can be either Gram-positive or Gram-negative, differentiated by their cell wall structure and reaction to Gram staining. Gram-negative coccobacilli often cause respiratory and zoonotic infections, while Gram-positive species are frequently associated with foodborne illnesses and genital infections.
Characteristics
They share several unique structural and functional traits that help classify and identify them in clinical microbiology.
Shape and Size Description
They are generally 0.5–1.0 µm wide and 1.0–2.0 µm long. Their short, oval form provides an evolutionary advantage in attaching to host tissues and surviving in varying environmental niches.
Cell Wall Structure
Like other bacteria, coccobacilli have a peptidoglycan-rich cell wall. In Gram-negative types, this is accompanied by an outer membrane containing lipopolysaccharides, contributing to antibiotic resistance and immune evasion.
Gram-positive coccobacilli lack this outer membrane but possess a thick peptidoglycan layer, aiding in resilience to environmental stresses.
Staining Properties
They display distinct staining patterns on Gram staining, crucial for preliminary identification. Gram-negative coccobacilli stain pink due to their thin peptidoglycan layer, while Gram-positive types appear purple.
Some species, such as Acinetobacter, may exhibit variable staining, complicating their interpretation in clinical samples.
Growth Requirements and Conditions
They have diverse nutritional and environmental requirements. Some are fastidious, requiring enriched media like chocolate agar (e.g., Haemophilus influenzae), while others, such as Acinetobacter, grow readily on ordinary nutrient media.
Temperature preferences also vary, with most pathogenic species thriving at human body temperature (37°C).
Pathogenicity and Virulence Factors
Many coccobacilli possess virulence mechanisms including capsules, exotoxins, endotoxins, and immune-modulating proteins. These factors allow them to invade host tissues, evade immune defenses, and cause disease.
For example, Bordetella pertussis produces pertussis toxin, contributing to whooping cough’s clinical manifestations.
Classification
They are classified using multiple criteria including Gram reaction, oxygen requirement, and pathogenic potential. These classifications aid in laboratory identification and treatment planning.
Based on Gram Staining
They are first divided into Gram-positive and Gram-negative categories based on their cell wall structure. This distinction is essential for determining antibiotic susceptibility and pathogenic behavior.
Based on Oxygen Requirement (Aerobic vs. Anaerobic)
Some coccobacilli require oxygen for growth (aerobes), while others grow in its absence (anaerobes) or in low-oxygen conditions (facultative anaerobes). This classification influences their growth media and incubation requirements.
Based on Pathogenic Potential
Clinically, coccobacilli are categorized as either pathogenic or commensal/environmental. Pathogenic species cause infections in humans and animals, while non-pathogenic types exist harmlessly in soil, water, and skin.
Common Gram-Negative Coccobacilli Examples
Several medically significant Gram-negative coccobacilli are responsible for respiratory, zoonotic, and hospital-acquired infections.
Haemophilus influenzae
A fastidious bacterium causing meningitis, epiglottitis, and otitis media in children. Requires X (hemin) and V (NAD) factors for growth.
Bordetella pertussis
Etiological agent of whooping cough. Produces pertussis toxin and filamentous hemagglutinin, contributing to prolonged respiratory symptoms.
Brucella Species
Causes brucellosis, a zoonotic infection acquired through contact with infected animals. Leads to undulant fever, joint pain, and malaise.
Francisella tularensis
Highly virulent, causing tularemia in humans, typically through tick bites or contact with infected animals. Requires cysteine-enriched media for laboratory growth.
Acinetobacter baumannii
An opportunistic, multidrug-resistant hospital pathogen causing pneumonia, bloodstream infections, and wound infections, particularly in ICU settings.
Common Gram-Positive Coccobacilli Examples
Though less numerous, several Gram-positive coccobacilli are clinically important, often causing foodborne and genital tract infections.
Listeria monocytogenes
A facultative intracellular pathogen responsible for listeriosis. Notable for its ability to grow at refrigeration temperatures and cross the placental barrier.
Gardnerella vaginalis
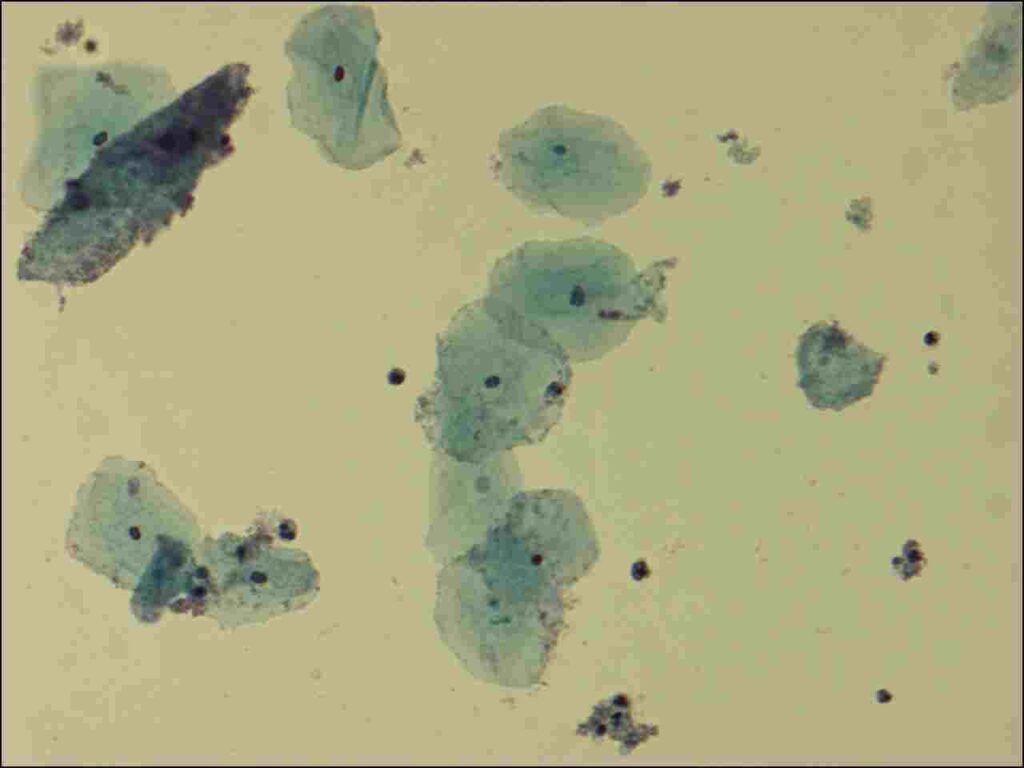
Involved in bacterial vaginosis. Characterized by a clue-cell formation on vaginal smear and a fishy odor due to amine production.
Actinomyces Species
Anaerobic or microaerophilic bacteria causing actinomycosis, a chronic granulomatous infection of soft tissues.
Clinical Significance
It play a significant role in human infectious diseases, with several species capable of causing serious illnesses. These bacteria are responsible for a wide range of clinical conditions, including respiratory infections, sexually transmitted diseases, zoonotic infections, and hospital-acquired infections.
Prompt identification and targeted treatment are vital, as many coccobacilli exhibit varying degrees of antibiotic resistance and rapid progression in clinical cases.
Coccobacilli in Respiratory Infections
Gram-negative coccobacilli like Haemophilus influenzae and Bordetella pertussis are prominent causes of respiratory tract infections. H. influenzae can lead to pneumonia, bronchitis, and life-threatening conditions like epiglottitis and meningitis in children.
Bordetella pertussis causes whooping cough, a highly contagious disease characterized by severe coughing fits that can result in respiratory distress, particularly in infants.
Coccobacilli in Zoonotic Diseases
Zoonotic infections, transmitted from animals to humans, often involve coccobacilli like Brucella and Francisella tularensis. These bacteria cause brucellosis and tularemia, respectively both of which are occupational hazards for veterinarians, farmers, and laboratory workers.
These infections typically present with non-specific symptoms like fever and fatigue but can progress to chronic and debilitating disease if untreated.
Role in Genitourinary Tract Infections
Some Gram-positive coccobacilli, such as Gardnerella vaginalis, are implicated in bacterial vaginosis, a common vaginal infection in women. It is characterized by abnormal discharge, odor, and altered vaginal flora.
Other species, like Listeria monocytogenes, though more commonly associated with foodborne illnesses, can also cause intrauterine infections and neonatal sepsis.
Nosocomial Infections and Antibiotic Resistance
Hospital-acquired infections, particularly those caused by Acinetobacter baumannii, pose a growing concern in healthcare settings. This opportunistic coccobacillus has developed resistance to multiple antibiotics, complicating treatment and increasing morbidity and mortality rates in immunocompromised and critically ill patients.
Infection control measures and antimicrobial stewardship are essential to limit the spread of these multidrug-resistant strains.
Laboratory Identification
Accurate laboratory identification of coccobacilli is critical for effective patient management and epidemiological surveillance. Multiple microbiological and molecular techniques are employed to confirm their presence and determine antimicrobial susceptibility.
Microscopy and Gram Staining
The first step in identifying coccobacilli involves direct microscopic examination of clinical samples stained by the Gram stain technique. This distinguishes between Gram-positive and Gram-negative coccobacilli based on cell wall properties.
They typically appear as short, oval, or slightly elongated rods arranged singly or in pairs, providing valuable preliminary diagnostic clues.
Culture Characteristics
They exhibit varying culture requirements depending on the species. Fastidious organisms like H. influenzae and F. tularensis require enriched media (e.g., chocolate agar) supplemented with specific growth factors or cysteine.
Non-fastidious species like Acinetobacter baumannii grow readily on blood agar and MacConkey agar, forming smooth, opaque colonies that aid in identification.
Biochemical Identification Tests
Biochemical assays are performed to further characterize coccobacilli based on their metabolic activities. Tests such as oxidase, catalase, urease, and carbohydrate fermentation profiles help differentiate species.
Automated systems like VITEK 2 and conventional biochemical panels provide reliable identification of coccobacilli in clinical laboratories.
Molecular Methods (PCR, MALDI-TOF MS)
Modern molecular techniques offer rapid and accurate identification of coccobacilli directly from clinical specimens. Polymerase Chain Reaction (PCR) amplifies specific genetic markers, while MALDI-TOF Mass Spectrometry profiles bacterial proteins for precise species-level identification.
These methods are particularly useful for identifying fastidious or slow-growing species that are difficult to culture.
Diseases Caused by them
They are responsible for several serious human diseases, many of which have high morbidity and mortality if not treated promptly. Early diagnosis and targeted therapy are essential for favorable outcomes.
Meningitis
Haemophilus influenzae type b (Hib) is a leading cause of bacterial meningitis in children under five years old. Before the advent of the Hib vaccine, it was responsible for thousands of deaths annually. Prompt antimicrobial therapy and supportive care are critical.
Whooping Cough
Bordetella pertussis causes whooping cough, an infectious respiratory disease marked by severe coughing fits followed by a characteristic “whoop” sound during inspiration. It is especially dangerous in infants, with complications including pneumonia, seizures, and death.
Brucellosis
A zoonotic infection caused by various Brucella species, brucellosis presents with undulating fever, night sweats, joint pain, and malaise. Chronic cases can result in endocarditis, osteomyelitis, and reproductive complications.
Tularemia
Caused by Francisella tularensis, tularemia is a rare but potentially severe infection transmitted through tick bites, inhalation, or contact with infected animals. Clinical forms include ulceroglandular, pneumonic, and typhoidal tularemia.
Listeriosis
Listeria monocytogenes causes listeriosis, a foodborne illness especially dangerous for pregnant women, neonates, the elderly, and immunocompromised individuals. It can lead to sepsis, meningitis, and fetal loss if untreated.
Treatment and Management
Managing coccobacilli infections involves antimicrobial therapy tailored to the specific organism and its resistance pattern. Early initiation of treatment is vital, particularly in severe and invasive infections.
Commonly Used Antibiotics
Standard antibiotics include ampicillin, ceftriaxone, doxycycline, gentamicin, and fluoroquinolones, depending on the organism and clinical scenario. Listeria, for example, is inherently resistant to cephalosporins, requiring ampicillin or penicillin-based regimens.
Challenges of Antibiotic Resistance
Multidrug resistance, particularly in Acinetobacter baumannii, poses a significant clinical challenge. Carbapenem-resistant strains limit therapeutic options and necessitate combination therapy or the use of last-resort agents like colistin.
Antimicrobial stewardship and infection control practices are critical to curb resistance development and transmission.
Vaccines for Prevention
Vaccines are available for certain coccobacilli-related infections. The Hib vaccine has drastically reduced meningitis and epiglottitis incidence worldwide. A vaccine against pertussis is included in the DTaP immunization schedule.
No vaccines are currently licensed for human brucellosis, tularemia, or listeriosis, though research efforts continue.
Recent Advances in their Research
Ongoing research has improved our understanding of coccobacilli pathogenesis, diagnostics, and treatment options. Technological advancements have enhanced the detection of fastidious and drug-resistant species.
Genomic Sequencing
Whole genome sequencing (WGS) of coccobacilli has unveiled critical virulence genes, resistance mechanisms, and transmission patterns. WGS is now increasingly integrated into epidemiological investigations and outbreak management.
New Diagnostic Techniques
Advances in rapid diagnostic tests like PCR-based multiplex assays and next-generation sequencing (NGS) have reduced turnaround times for pathogen identification and resistance profiling.
Molecular point-of-care testing holds promise for the early detection of life-threatening coccobacilli infections.
Emerging Drug-Resistant Strains
The emergence of extensively drug-resistant (XDR) Acinetobacter baumannii and resistant strains of Listeria and Brucella has raised global health concerns. Surveillance programs and novel antimicrobial development are vital to addressing this issue.
Preventive Strategies
Preventing coccobacilli infections requires a combination of public health measures, vaccination, and strict infection control practices in healthcare and community settings.
Infection Control in Healthcare Settings
Standard precautions, hand hygiene, patient isolation, and environmental cleaning are essential to prevent hospital-acquired infections by coccobacilli like Acinetobacter baumannii.
Strict adherence to antimicrobial stewardship policies helps limit unnecessary antibiotic use and resistance emergence.
Public Health Surveillance Programs
Active surveillance of zoonotic diseases and respiratory infections aids in early detection and containment of outbreaks. Reporting systems and coordinated public health responses reduce morbidity and mortality associated with coccobacilli infections.
Conclusion
Coccobacilli represent a clinically diverse group of bacteria responsible for numerous human infections ranging from mild illnesses to severe, life-threatening diseases. Their varied morphology, growth requirements, and resistance patterns pose diagnostic and therapeutic challenges.
Early identification through microscopy, culture, and molecular techniques, coupled with appropriate antimicrobial therapy, remains the cornerstone of effective management. Continued research, public health vigilance, and infection control efforts are essential to combat the rising threat of antimicrobial resistance and emerging pathogens within this important bacterial group.
Frequently Asked Questions (FAQ)
What distinguishes coccobacilli from other bacteria?
They are short, oval-shaped bacteria with a morphology intermediate between spherical cocci and rod-shaped bacilli, making them unique in appearance under the microscope.
Are coccobacilli dangerous?
Yes, several coccobacilli species cause serious diseases like meningitis, whooping cough, listeriosis, and hospital-acquired infections, some with high morbidity if untreated.
How are coccobacilli diagnosed in the lab?
They are diagnosed using Gram staining, culture on selective media, biochemical tests, and modern molecular techniques like PCR and MALDI-TOF MS.
Related Contents
Coagulase Test- Principle, Procedure, Types, Result, Uses
Clostridium perfringens: Overview, Enterotoxins and Food Poisoning