Introduction
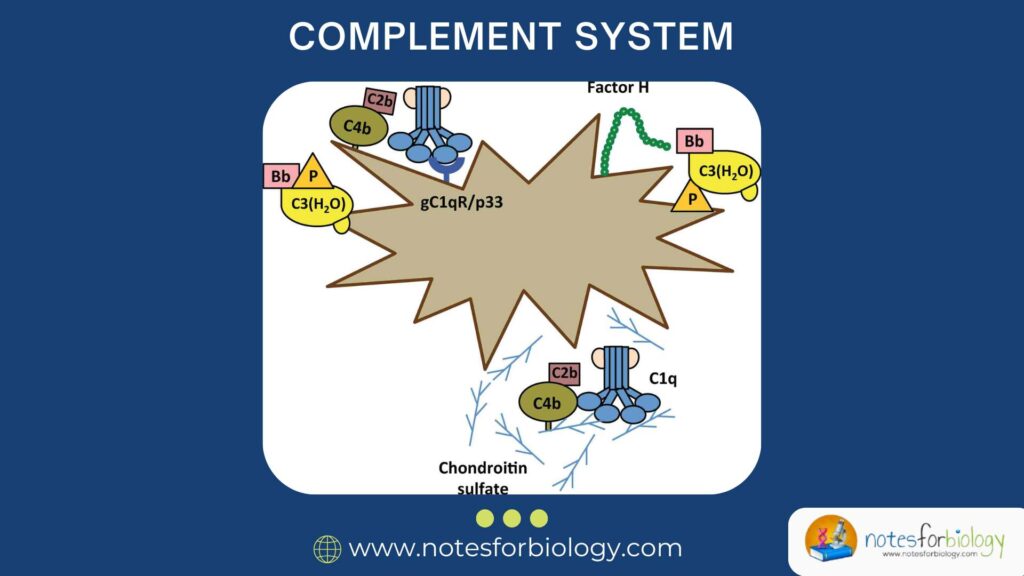
The complement system is one of the most powerful parts of our body’s immune defense. It consists of a group of proteins that work together to protect us from infections, clean up damaged cells, and support other parts of the immune system. While its functions are fascinating, understanding its properties and naming system (nomenclature) is equally important for grasping how this system works in health and disease.
Table of Contents
What is the Complement System?
Definition:
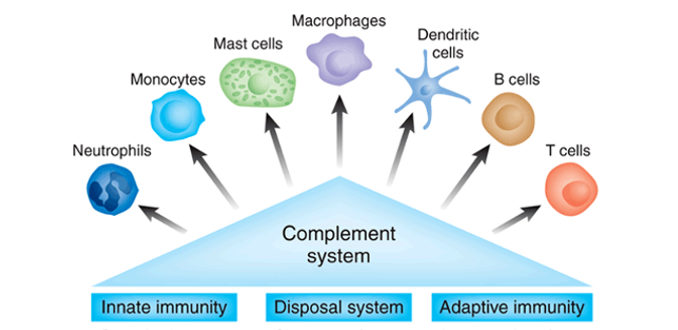
The complement system is a network of more than 30 proteins found in blood plasma and on cell surfaces. These proteins are part of the innate immune system and can be activated to respond quickly to pathogens such as bacteria, viruses, and fungi.
Once activated, the complement system performs several functions:
- Destroys microbes directly by forming holes in their membranes
- Tags invaders for destruction by immune cells
- Triggers inflammation to recruit more immune cells
- Clears damaged or dead cells from the body
Properties of Complement System
The complement system has several key properties that make it unique, powerful, and tightly controlled.
1. Activation by Cascading Mechanism
Complement proteins are activated in a cascade, meaning one component activates the next in a sequence.
- This allows for rapid and amplified responses.
- A small trigger can result in a large immune response.
2. Three Activation Pathways
The complement system can be activated in three different ways:
- Classical Pathway – triggered by antibodies bound to antigens
- Alternative Pathway – triggered directly by pathogen surfaces
- Lectin Pathway – triggered by sugar molecules on microbial surfaces
All three pathways eventually converge at the activation of C3, a central protein in the cascade.
3. Enzyme Amplification
Complement activation involves enzyme complexes like C3 convertase and C5 convertase that split other complement proteins into smaller fragments.
- These enzymes amplify the response quickly.
- Each step produces more active fragments that continue the chain reaction.
4. Irreversible Activation
Once complement proteins are activated, the process cannot be reversed.
- The system must be tightly regulated to prevent damage to healthy cells.
5. Host Cell Protection
The body has built-in regulatory proteins (e.g., Factor H, CD59) that prevent complement from attacking its own cells.
- This ensures specificity toward harmful invaders and avoids autoimmunity.
6. Lytic and Non-Lytic Functions
Complement proteins can:
- Lyse (burst) pathogens through membrane attack complex (MAC)
- Signal other immune responses, such as inflammation or opsonization
7. Heat-Labile Nature
Complement proteins are heat-sensitive.
- Heating serum at 56°C for 30 minutes can inactivate the complement system.
- This property is used in laboratory testing to prepare complement-free serum.
8. Short Half-Life
Once activated, many complement proteins are only active for a short period.
- This ensures that the response is localized and controlled.
Complement System: Nomenclature
Why Nomenclature is Important
Understanding how complement components are named helps in grasping how they function and interact with each other. The nomenclature may seem confusing at first, but once you understand the logic, it becomes easier.
General Rules of Complement Nomenclature
- Main components are designated by the letter “C” followed by a number (e.g., C1, C2, C3, etc.).
- When a component is activated, it is split into:
- A smaller fragment, usually labeled “a” (e.g., C3a)
- A larger fragment, usually labeled “b” (e.g., C3b)
- Some components are named based on their function or origin, not numerically.
- Properdin – a stabilizer of the alternative pathway
- Factor B, Factor D – enzymes in the alternative pathway
- Mannose-Binding Lectin (MBL) – a protein in the lectin pathway
- Regulatory proteins have their own specific names:
- Factor H, Factor I – inhibitors
- DAF (Decay Accelerating Factor) – protective for host cells
- CD59 – prevents MAC formation on host cells
Classical Complement Components (C1 to C9)
These components are the traditional series involved in the classical pathway.
1. C1 Complex
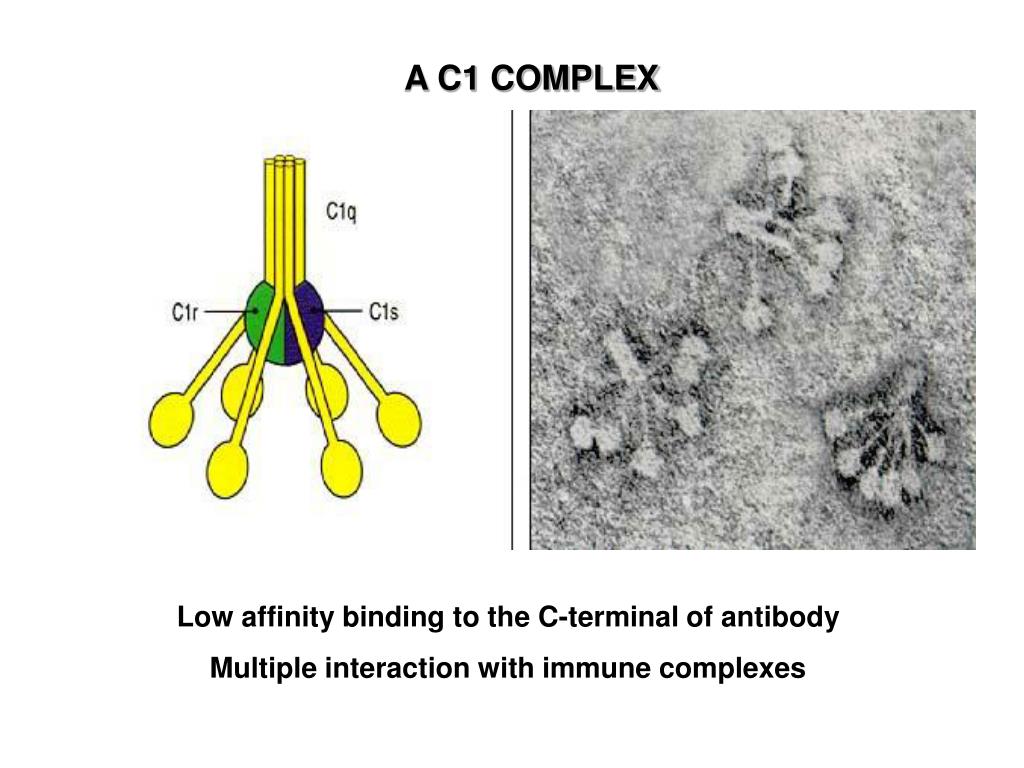
- Made of C1q, C1r, and C1s
- Initiates the classical pathway when C1q binds to antibodies on a pathogen
2. C2 and C4
- Cleaved into C2a, C2b, C4a, C4b after activation
- Form part of C3 convertase (C4b2a)
3. C3
- Central to all pathways
- Cleaved into:
- C3a – promotes inflammation (anaphylatoxin)
- C3b – opsonin; binds to pathogens to mark them for destruction
4. C5 to C9
- Form the Membrane Attack Complex (MAC)
- MAC creates pores in the pathogen membrane leading to cell lysis
Special Note:
For C2, the larger fragment is C2a, which is different from the naming rule (where “b” is usually larger).
Alternative Pathway Components
These are components specific to the alternative pathway.
1. Factor B
- Binds to C3b on microbial surfaces
- Cleaved by Factor D into Ba and Bb
- Bb forms part of the alternative pathway C3 convertase (C3bBb)
2. Factor D
- A serine protease
- Cleaves Factor B
3. Properdin (P)
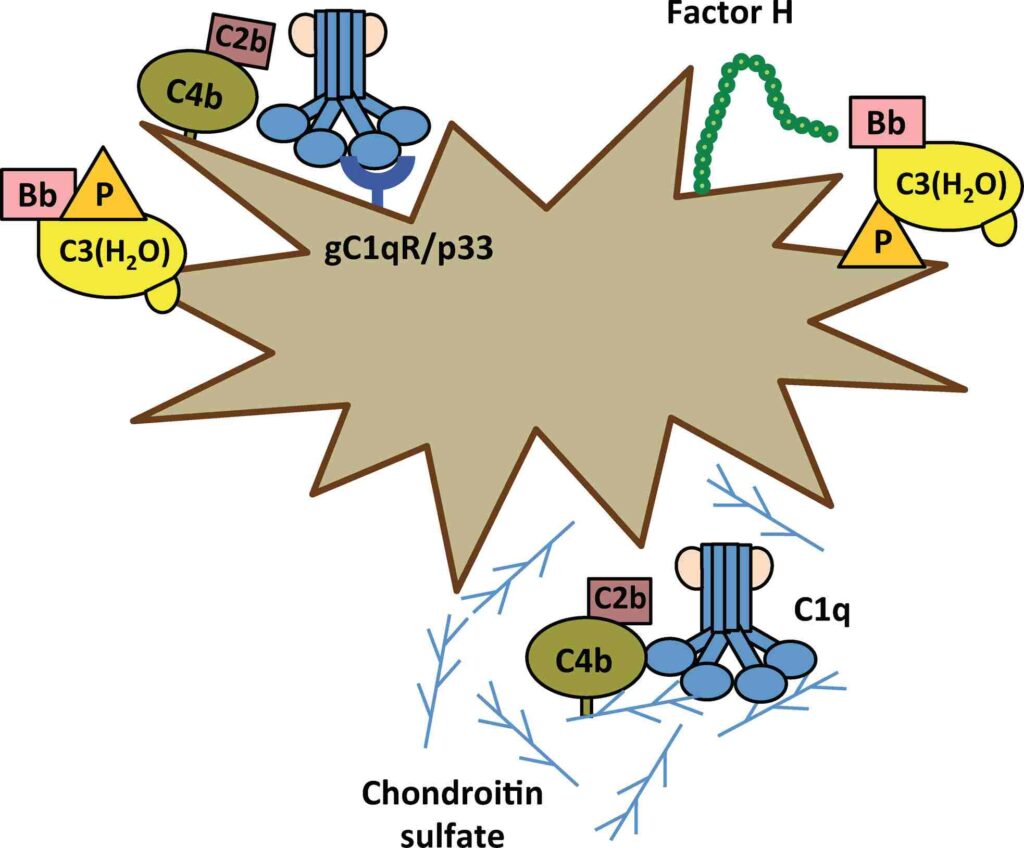
- Stabilizes the alternative pathway C3 convertase
- Unique because it is a positive regulator
Lectin Pathway Components
1. Mannose-Binding Lectin (MBL)
- Binds to carbohydrate residues on microbial surfaces
- Activates MBL-Associated Serine Proteases (MASPs)
2. MASP-1 and MASP-2
- Cleave C4 and C2 to form C3 convertase, similar to the classical pathway
Anaphylatoxins: C3a, C4a, C5a
These fragments are powerful chemical messengers:
- Increase blood vessel permeability
- Attract immune cells to the site of infection (chemotaxis)
- Stimulate release of histamine
Among them, C5a is the most potent in causing inflammation.
Complement Regulatory Proteins
These proteins prevent overactivation and protect host cells:
1. Factor H and Factor I
Inhibit C3 convertase in the alternative pathway
2. DAF (Decay Accelerating Factor)
Breaks down convertases on human cells
3. CD59 (Protectin)
Prevents MAC formation on host cell membranes
Receptors for Complement Components
Immune cells have specific receptors for recognizing activated complement fragments.
Common Receptors:
- CR1 (CD35) – binds to C3b, helps with opsonization
- CR2 (CD21) – binds to C3d; helps B cell activation
- CR3 and CR4 – help in cell adhesion and phagocytosis
Common Abbreviations in Complement Nomenclature
| Abbreviation | Full Name / Meaning |
|---|---|
| C3, C4, C5 | Complement proteins |
| C3a, C5a | Small fragments involved in inflammation |
| C3b, C4b | Larger fragments that bind pathogens |
| MAC | Membrane Attack Complex (C5b-C9) |
| DAF | Decay Accelerating Factor |
| MBL | Mannose-Binding Lectin |
| CR1-CR4 | Complement Receptors |
| P | Properdin |
Conclusion
The complement system is a powerful part of our immune defense that relies on a delicate balance of activation and regulation. To fully appreciate its role, one must understand not only what the complement proteins do but also how they are organized and named. The complement nomenclature may seem complex at first, but it follows a logical pattern based on the protein’s function, sequence of activation, and role in different pathways.
Through the classical, alternative, and lectin pathways, the complement system coordinates a swift and targeted response against threats — from tagging pathogens for destruction to blowing holes in them with the membrane attack complex. Knowing the properties and naming rules of this system helps us better understand how our body defends itself and how researchers develop treatments for immune-related diseases.
FREQUENTLY ASKED QUESTIONS
Why is it called the “complement” system?
Because it “complements” (enhances) the ability of antibodies and other immune cells to fight infections.
What does “C3b” mean?
It is the larger fragment formed when the C3 protein is cleaved. It binds to pathogens and marks them for destruction.
What happens if complement is not regulated?
It can damage the body’s own tissues, leading to autoimmune or inflammatory diseases.
Related Articles