The chambers of the heart are the four internal spaces through which blood flows, allowing the heart to pump blood effectively throughout the body. These chambers include two atria (also called auricles) at the top and two ventricles at the bottom.
The human heart is an extraordinary muscular organ that serves as the central pump of the circulatory system. It beats continuously, propelling blood throughout the body to deliver oxygen and essential nutrients to cells while removing carbon dioxide and waste products. A fundamental aspect of this pump system is the heart’s internal architecture specifically, the four chambers that coordinate blood flow through the lungs and body. These chambers include two auricles (also known as atria) and two ventricles. Each plays a unique and essential role in maintaining circulation and overall health. This expanded article provides an in-depth look at the structure, function, and clinical significance of these chambers.
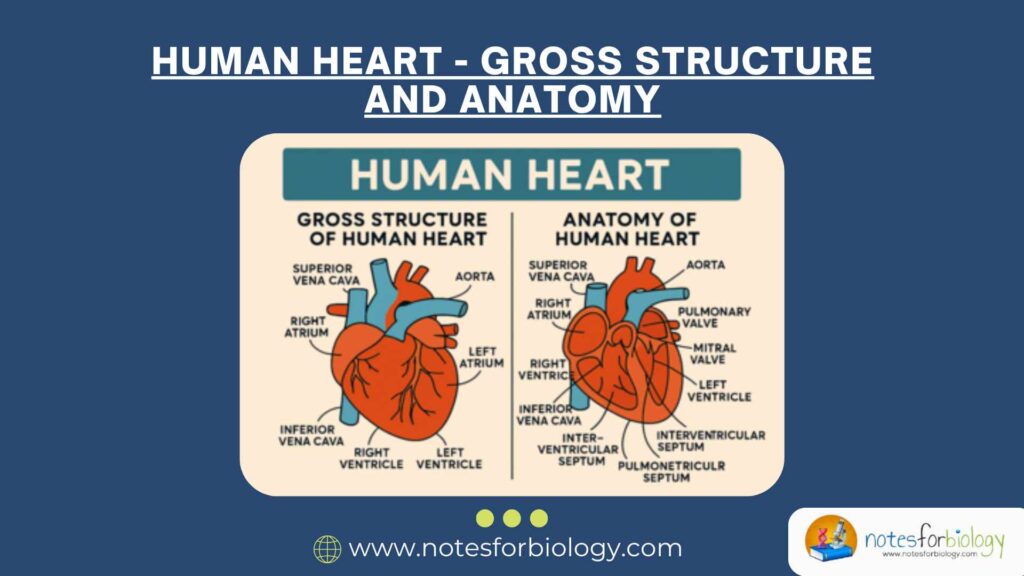
1. Introduction to the Heart’s Chambers
The human heart is divided into four chambers:
- Right Atrium (Right Auricle)
- Right Ventricle
- Left Atrium (Left Auricle)
- Left Ventricle
The upper chambers, the atria (auricles), are primarily responsible for receiving blood returning to the heart. The lower chambers, the ventricles, pump blood away from the heart to the lungs for oxygenation or to the rest of the body. The chambers work in a highly synchronized fashion, contracting and relaxing in a coordinated cycle to ensure continuous and efficient blood flow. Valves and walls, known as septa, separate the chambers and prevent the backward flow of blood.
Summary of Chambers of Heart
| Chamber | Function | Blood Type | Connected Vessels |
|---|---|---|---|
| Right Atrium | Receives blood from the body | Deoxygenated | Superior & Inferior Vena Cava |
| Right Ventricle | Sends blood to the lungs | Deoxygenated | Pulmonary Artery |
| Left Atrium | Receives blood from the lungs | Oxygenated | Pulmonary Veins |
| Left Ventricle | Sends blood to the body | Oxygenated | Aorta |
Table of Contents
2. Auricles (Atria)
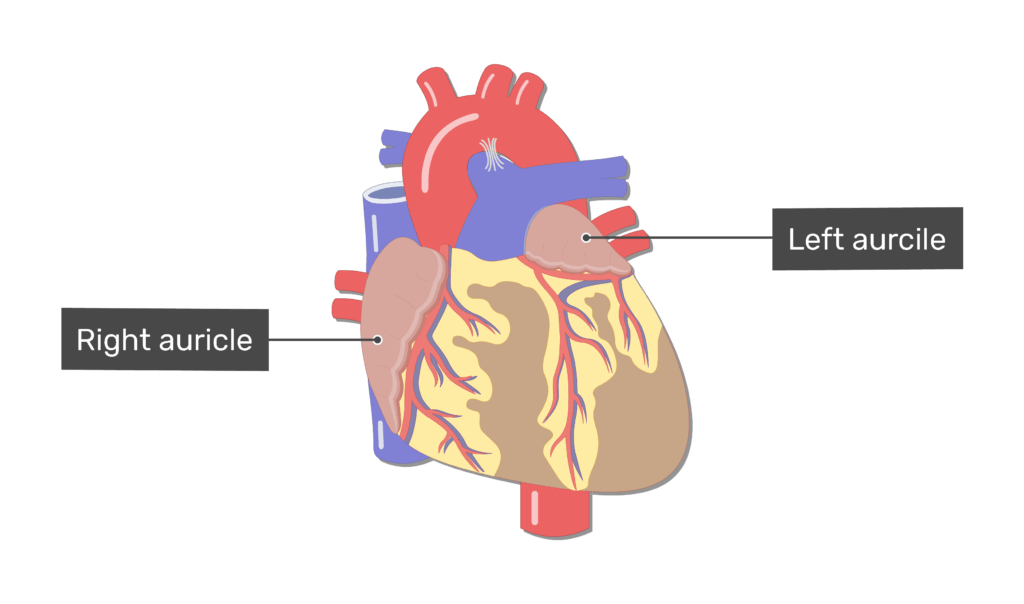
The auricles are the heart’s thin-walled, upper chambers. Although relatively small, they play an essential role by receiving blood from the veins and passing it to the ventricles.
2.1 Right Auricle (Right Atrium)
- Function: Acts as the entry point for deoxygenated blood coming from the body. It collects blood from the superior vena cava (draining the upper body), the inferior vena cava (draining the lower body), and the coronary sinus (draining the heart muscle itself).
- Structure: Thin and expandable, the right auricle helps accommodate varying volumes of blood. It has a small muscular pouch that increases its capacity.
- Additional Features: Contains the sinoatrial (SA) node, which generates electrical impulses that initiate each heartbeat. This makes it the natural pacemaker of the heart.
2.2 Left Auricle (Left Atrium)
- Function: Receives oxygen-rich blood from the lungs through four pulmonary veins (two from each lung). It holds and passes this blood to the left ventricle.
- Structure: Slightly thicker walls than the right atrium due to the increased pressure of pulmonary circulation. Also has an auricular appendage to increase capacity.
- Importance: Acts as a transitional chamber to ensure that oxygenated blood is efficiently transferred to the left ventricle for distribution throughout the body.
3. Ventricles
The ventricles are the lower, muscular chambers of the heart. They have thicker walls than the auricles because they must generate the force necessary to push blood either to the lungs or to the rest of the body.
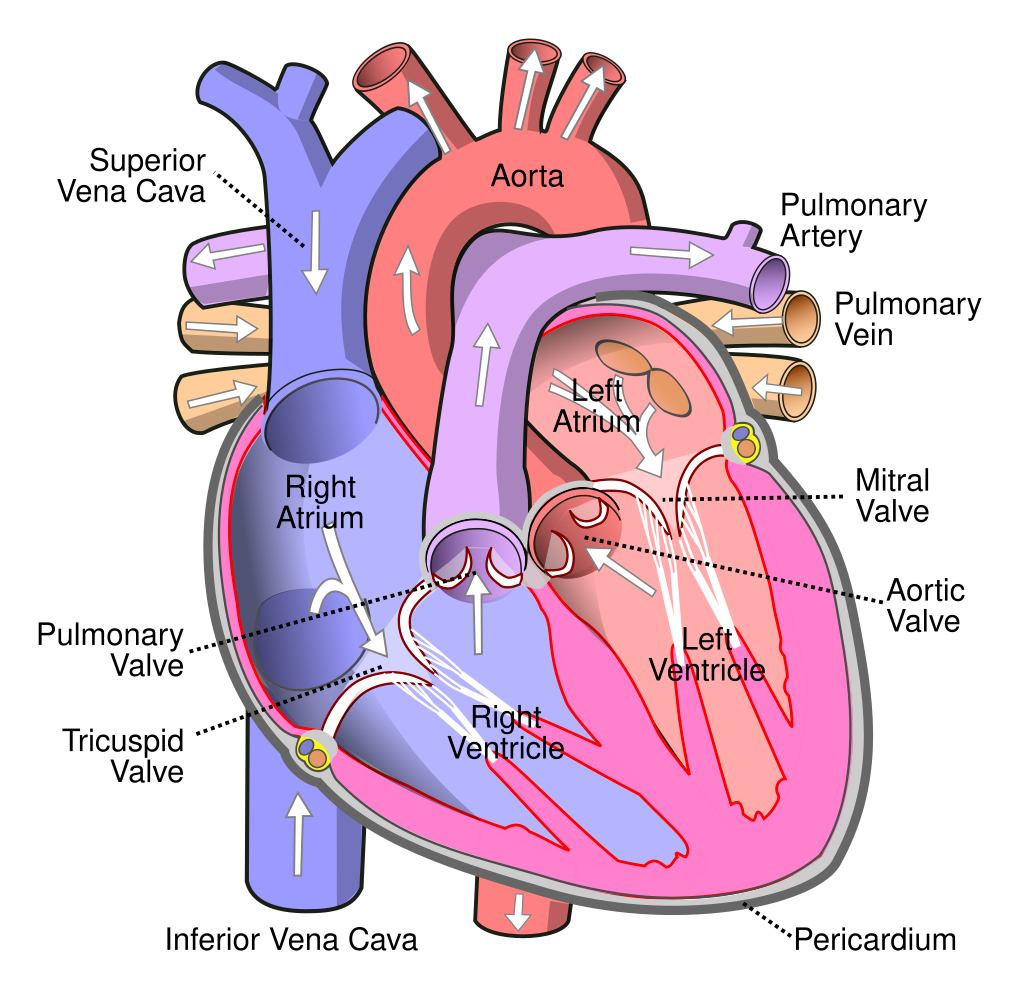
3.1 Right Ventricle
- Function: Pumps deoxygenated blood from the right atrium to the lungs via the pulmonary artery, where the blood becomes oxygenated.
- Structure: Has a crescent-shaped cavity and moderately thick muscular walls. The pressure here is lower compared to the left ventricle since it only pumps blood to the nearby lungs.
- Valves: Blood enters the right ventricle from the right atrium through the tricuspid valve and exits to the pulmonary artery through the pulmonary valve.
3.2 Left Ventricle
- Function: Pumps oxygen-rich blood from the left atrium to the entire body through the aorta.
- Structure: Has the thickest walls of all the heart chambers, as it must create high pressure to move blood throughout the systemic circulation.
- Valves: Receives blood through the mitral (bicuspid) valve and pumps it into the aorta through the aortic valve.
4. Valves and Septa Between Chambers
To maintain one-way blood flow, the heart includes four valves and two main septa:
- Tricuspid Valve: Controls blood flow from the right atrium to the right ventricle.
- Pulmonary Valve: Allows blood to flow from the right ventricle into the pulmonary artery and prevents backflow.
- Mitral (Bicuspid) Valve: Regulates blood flow from the left atrium to the left ventricle.
- Aortic Valve: Controls the flow of oxygenated blood from the left ventricle into the aorta.
- Interatrial Septum: The wall between the left and right atria, preventing mixing of oxygenated and deoxygenated blood.
- Interventricular Septum: The thick muscular wall between the left and right ventricles, essential for coordinated contraction.
5. Blood Flow Through the Heart
The flow of blood through the heart follows a specific and efficient path:
- Deoxygenated blood enters the right atrium from the superior and inferior vena cava.
- It flows through the tricuspid valve into the right ventricle.
- The right ventricle pumps it through the pulmonary valve into the pulmonary artery.
- Blood travels to the lungs, where it picks up oxygen and releases carbon dioxide.
- Oxygenated blood returns to the left atrium via the pulmonary veins.
- It then flows through the mitral valve into the left ventricle.
- The left ventricle pumps the oxygen-rich blood through the aortic valve into the aorta, distributing it to the entire body.
This cycle ensures that oxygen-poor blood is re-oxygenated in the lungs and that oxygen-rich blood is circulated to all tissues.
6. Electrical Conduction System
The heart’s rhythm and coordination are controlled by an intrinsic electrical conduction system:
- Sinoatrial (SA) Node: Located in the right atrium, it acts as the primary pacemaker, setting the pace of the heartbeat.
- Atrioventricular (AV) Node: Receives the impulse from the SA node and delays it slightly to ensure the atria contract before the ventricles.
- Bundle of His: Transmits impulses from the AV node to the ventricles.
- Purkinje Fibers: Spread throughout the ventricular walls, these fibers cause the ventricles to contract in a synchronized manner.
This conduction system ensures that the atria contract first, followed by the ventricles, allowing efficient blood movement
7. Clinical Relevance of Heart Chambers
- Heart Failure: May involve one or both ventricles, leading to insufficient blood circulation. Left-sided failure affects systemic circulation, while right-sided failure leads to fluid accumulation in tissues.
- Atrial Fibrillation (AFib): A common arrhythmia originating in the atria, leading to irregular and often rapid heartbeats, increasing the risk of stroke.
- Ventricular Hypertrophy: Thickening of the ventricular walls, often due to high blood pressure or valvular heart disease, which can reduce pumping efficiency.
- Septal Defects: Congenital abnormalities like atrial septal defect (ASD) or ventricular septal defect (VSD) allow abnormal blood flow between chambers, potentially causing oxygen level imbalances and heart strain.
8. Diagnostic Tools
- Echocardiogram: An ultrasound test that creates images of the heart chambers, valves, and motion to assess structure and function.
- ECG/EKG (Electrocardiogram): Measures the electrical activity of the heart to detect arrhythmias, heart attacks, and other abnormalities.
- MRI and CT Scans: Provide high-resolution, 3D images of heart anatomy for detailed assessment.
- Cardiac Catheterization: Involves inserting a catheter into the heart to measure pressure, blood flow, and chamber functionality.
These tools help diagnose and monitor diseases affecting the heart chambers and guide treatment decisions.
9. Conclusion
The auricles and ventricles of the heart work together in a precisely coordinated manner to maintain life. The auricles receive incoming blood, while the ventricles deliver it forcefully to the lungs or the entire body. This collaboration ensures the efficient delivery of oxygen and nutrients and the removal of waste products. Any disruption in this system can have serious consequences, highlighting the importance of maintaining heart health. Understanding each chamber’s role helps in appreciating how the heart functions and in recognizing signs of disease early for prompt intervention.
Frequently Asked Questions (FAQs)
What is the function of the atrium?
An atrium is a thin-walled, “receiving” chamber. The right atrium brings oxygen-poor blood from the body, and the left atrium brings oxygen-rich blood from the lungs. They act as holding rooms before blood moves into the stronger ventricles .
What is the function of the ventricle?
Ventricles are muscular “pumping” chambers. The right ventricle sends blood to the lungs to pick up oxygen, while the left ventricle pumps blood into the aorta for distribution to the entire body. They work harder than atria because they move blood under higher pressure .
How does blood flow through the heart?
Blood enters the right atrium from the body, moves to the right ventricle, and is pumped to the lungs. Oxygen-rich blood returns to the left atrium, flows into the left ventricle, and is finally pumped out through the aorta to the body. This ensures fresh oxygen is constantly supplied.
Related Articles