Fungal pathogens have increasingly become a prominent concern in clinical microbiology due to their capacity to cause a broad spectrum of diseases. Among these, Candida tropicalis stands out as a significant opportunistic yeast responsible for both superficial and systemic infections. Notably, this pathogen is particularly dangerous for immunocompromised patients, including those with neutropenia, cancer, or undergoing organ transplants. Its emerging antifungal resistance also places it at the forefront of fungal pathogens warranting global attention.
Over the past few decades, the frequency of Candida tropicalis infections has surged, particularly in tropical and subtropical regions like Southeast Asia and Latin America. This increase correlates with the growing population of immunosuppressed individuals and the widespread use of broad-spectrum antibiotics and invasive medical procedures, which disrupt normal flora and facilitate fungal overgrowth.
Summary of Candida tropicalis
- Candida tropicalis is an opportunistic yeast-like fungus commonly found as a commensal in the human gut and skin but capable of causing serious infections, especially in immunocompromised people.
- It forms biofilms, produces hydrolytic enzymes, and undergoes phenotypic switching, making it a key cause of superficial infections and invasive candidiasis, particularly in hospitalized patients.
- Diagnosis includes microscopy, culture, biochemical, and molecular methods, while treatment uses azoles, echinocandins, or amphotericin B, though rising antifungal resistance requires careful management and control.
Table of Contents
Definition and Classification
Candida tropicalis is a yeast-like opportunistic fungal pathogen classified under the kingdom Fungi. It belongs to the genus Candida, within the family Saccharomycetaceae. This species is one of the non-albicans Candida (NAC) group members increasingly implicated in healthcare-associated infections.
Taxonomic Classification of Candida tropicalis
The formal taxonomic hierarchy of C. tropicalis is as follows:
- Kingdom: Fungi
- Division: Ascomycota
- Class: Saccharomycetes
- Order: Saccharomycetales
- Family: Saccharomycetaceae
- Genus: Candida
- Species: Candida tropicalis
This classification places Candida tropicalis within the group of ascomycetous yeasts, distinguishing it from filamentous fungi and placing it alongside other important clinical yeasts. Its position within the Saccharomycetaceae family reflects its evolutionary and genetic relationships to other medically significant Candida species.
Opportunistic Nature
While it exists harmlessly as a commensal organism in healthy individuals, C. tropicalis can become pathogenic when host immunity is compromised. It transitions from a benign colonizer to an invasive pathogen, exploiting weakened defenses to cause superficial mucocutaneous infections or disseminated systemic diseases. This opportunistic behavior underscores the importance of maintaining immune system integrity and highlights the challenges faced in treating immunocompromised patients.
Morphology of Candida tropicalis
The morphological features of Candida tropicalis exhibit significant variability depending on environmental conditions and the organism’s physiological state. These morphological adaptations allow the organism to survive under different environmental pressures and during various stages of infection.
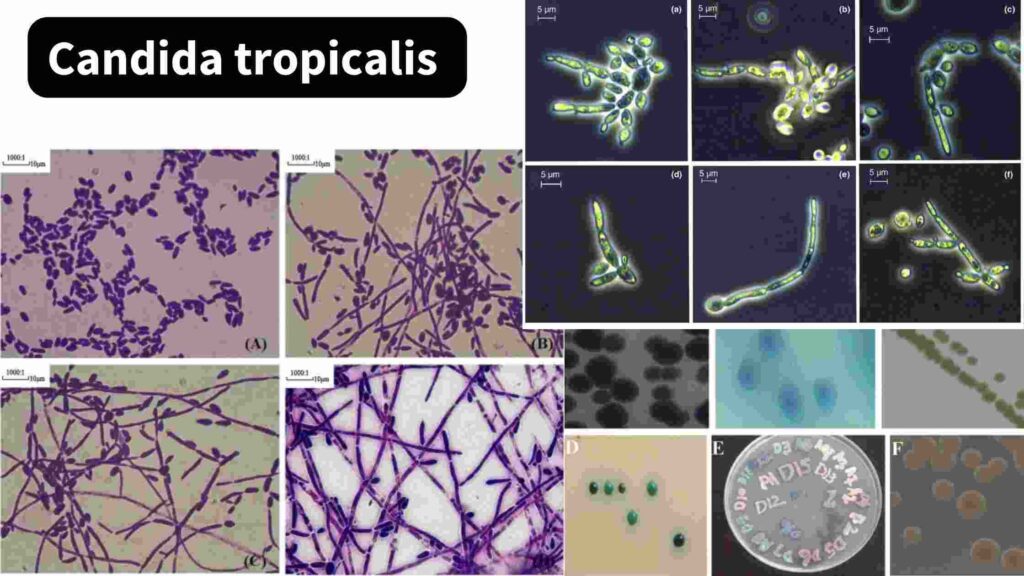
Yeast Form
In its yeast form, C. tropicalis appears as oval or spherical budding cells. These are typically visualized using light microscopy after Gram staining, where they exhibit Gram-positive, purple-colored appearances. This form predominates during its commensal existence within the human microbiome and serves as the initial stage from which more invasive forms can develop under suitable conditions.
Pseudohyphae and True Hyphae Formation
Under conditions conducive to infection, such as host tissue invasion, C. tropicalis transitions into filamentous forms, including pseudohyphae and true hyphae. Pseudohyphae consist of elongated chains of yeast cells with constrictions at their junctions, while true hyphae are continuous, septate filamentous structures. This morphological plasticity enhances its invasive capabilities and contributes to tissue penetration and biofilm formation, important aspects of its pathogenicity.
Colony Morphology
On solid culture media, C. tropicalis produces distinctive colony morphologies. On Sabouraud Dextrose Agar (SDA), colonies are smooth, creamy, and glistening. On CHROMagar Candida, a differential chromogenic medium, colonies of C. tropicalis typically exhibit a metallic dark blue color, facilitating presumptive species identification. These morphological characteristics aid clinical microbiologists in preliminary diagnosis before confirmatory tests are performed.
Habitat and Reservoirs
The ecological versatility of Candida tropicalis allows it to thrive in various environments, both within and outside the human body. Its ability to colonize multiple habitats contributes to its persistence and transmission potential.
Human Commensal
In humans, C. tropicalis colonizes the gastrointestinal tract, oral cavity, skin, and vaginal mucosa. Under normal circumstances, it exists as part of the commensal flora, regulated by the host immune system and competitive microbial species. Disruption of these regulatory mechanisms, as seen with antibiotic use or immunosuppression, can result in overgrowth and infection.
Environmental Distribution
Beyond the human host, C. tropicalis has been isolated from environmental sources including soil, decaying vegetation, marine and freshwater ecosystems, and animal excreta. This widespread distribution contributes to its indirect transmission and potential for causing opportunistic infections, especially in individuals exposed to contaminated environments or undergoing invasive medical procedures.
Nosocomial Reservoirs
Within healthcare settings, C. tropicalis can colonize surfaces, water sources, and medical equipment. It has been implicated in nosocomial outbreaks, particularly in intensive care units (ICUs) where invasive procedures and prolonged antibiotic use disrupt normal flora and facilitate fungal colonization. The presence of C. tropicalis on medical devices underscores the need for stringent infection control protocols in hospitals.
Pathogenicity and Virulence Factors
The pathogenic potential of Candida tropicalis arises from an array of virulence factors that facilitate adhesion, invasion, immune evasion, and biofilm formation. These attributes enable the organism to establish infection, persist within the host, and resist antifungal treatment.
Adhesion to Surfaces
Adhesion is a prerequisite for colonization and infection. C. tropicalis expresses surface adhesins that enable attachment to host epithelial cells and medical devices. This adhesion initiates colonization, biofilm development, and subsequent infection. Effective adhesion is crucial for survival within the host and the initiation of disease processes.
Biofilm Formation
Biofilms are structured communities of yeast cells embedded within an extracellular matrix. C. tropicalis biofilms exhibit enhanced resistance to antifungal agents and immune defenses, contributing to persistent infections, especially those associated with indwelling medical devices. Biofilm-associated infections are particularly difficult to treat and often necessitate device removal in addition to antifungal therapy.
Hydrolytic Enzyme Production
The organism produces several hydrolytic enzymes, including proteases, phospholipases, and hemolysins. Proteases degrade host tissue proteins, phospholipases disrupt cell membranes, and hemolysins lyse erythrocytes, providing iron for fungal growth. These enzymes play vital roles in tissue invasion, nutrient acquisition, and evasion of host immune responses.
Phenotypic Switching
Candida tropicalis can undergo phenotypic switching, altering its colony morphology and antigenic properties. This adaptability facilitates immune evasion and survival in varied environmental conditions. Phenotypic switching allows the organism to adjust to environmental stressors and host immune attacks, contributing to its persistence and pathogenicity.
Prevention and Control
The prevention and control of Candida tropicalis infections, particularly in healthcare environments, demand a multifaceted strategy focusing on infection control measures, patient monitoring, and public health awareness.
Infection Control in Healthcare Settings
Hospitals and intensive care units, where C. tropicalis often causes outbreaks, must enforce strict infection control protocols. This includes regular disinfection of surfaces, proper sterilization of medical equipment, and maintenance of aseptic techniques during invasive procedures. Limiting the unnecessary use of broad-spectrum antibiotics is also crucial, as these drugs disrupt the natural microbial flora, providing opportunities for fungal overgrowth.
Surveillance and Early Detection
Routine surveillance cultures and monitoring of high-risk patients can help detect colonization early. This facilitates timely intervention before progression to invasive disease. Monitoring antifungal susceptibility patterns in clinical isolates is equally important for guiding effective treatment, particularly given the emergence of azole resistance in C. tropicalis.
Patient Risk Reduction Measures
Patients with known risk factors, such as those undergoing chemotherapy, organ transplantation, or long-term ICU admission, should receive proactive care to minimize fungal colonization and infection. Measures include minimizing indwelling catheter use, maintaining skin integrity, and controlling blood glucose levels in diabetic patients.
Public Health Education
Raising awareness about fungal infections and their risk factors is vital, especially in endemic regions. Public health campaigns can educate healthcare workers, patients, and caregivers about the importance of hygiene, early symptom recognition, and adherence to prescribed antifungal therapies. This educational outreach contributes to lowering the incidence and transmission of Candida tropicalis infections.
Epidemiology
The epidemiological patterns of Candida tropicalis infections reveal its global presence with distinct regional variations. High prevalence rates are documented in Asia, Latin America, and parts of the Middle East, correlating with tropical and subtropical climates.
Global Prevalence
The incidence of candidemia and other systemic infections due to C. tropicalis has shown an upward trend globally, particularly in developing countries. Its ability to adapt to warm, humid environments and the widespread use of invasive medical procedures have contributed to its dominance in certain healthcare settings.
Risk Factor Associations
Epidemiological studies consistently link C. tropicalis infections with immunocompromised states, prolonged hospitalization, use of central venous catheters, and prior antibiotic therapy. Regional outbreaks have also been associated with lapses in infection control practices and contaminated hospital water systems.
Conclusion
Candida tropicalis is a medically significant fungal pathogen with the potential to cause a broad spectrum of diseases, ranging from superficial infections to life-threatening invasive candidiasis. Its capacity for biofilm formation, phenotypic switching, and hydrolytic enzyme production contributes to its virulence and complicates treatment outcomes.
Accurate identification, awareness of antifungal resistance trends, and adherence to infection control measures are key to managing infections caused by this opportunistic yeast. With its increasing prevalence, C. tropicalis demands vigilant clinical and laboratory attention in both community and healthcare settings.
Frequently Asked Questions (FAQ)
What is Candida tropicalis?
It’s an opportunistic yeast-like fungus found in humans, capable of causing serious infections in immunocompromised people.
How is Candida tropicalis diagnosed?
Diagnosis involves microscopy, culture, biochemical tests, and molecular techniques like PCR or MALDI-TOF.
Which antifungals treat Candida tropicalis infections?
Azoles, echinocandins, and amphotericin B are commonly used, chosen based on infection type and drug sensitivity.
Related Contents
Candida albicans- Taxonomy , Morphology, Habitat and Pathology
Campylobacter Blood Agar (CVA)- Composition, Principle, Preparation, Results, Uses