Candida albicans is a medically important fungal species that is both a normal resident of the human microbiota and a common opportunistic pathogen. It mainly inhabits mucosal surfaces, such as the mouth, gastrointestinal tract, and vagina, without causing harm under normal conditions. However, it can switch to a pathogenic form when the immune system is weakened or the normal microbial balance is disrupted.
The significance of Candida albicans in medicine arises from its ability to cause a variety of infections, ranging from mild superficial infections to potentially fatal systemic diseases. This overview explores its biology, morphology, pathogenic mechanisms, clinical relevance, diagnosis, treatment, and resistance issues.
Summary of Candida albicans
- Candida albicans is a common fungal pathogen found in the normal human flora.
- It can cause infections when immunity is low or the microbial balance is disturbed.
- Virulence factors like hyphae formation and biofilms help it invade and resist treatment.
Table of Contents
Taxonomy and Morphology
Understanding the classification and structural forms of Candida albicans is key to grasping its adaptability and pathogenicity.
Candida albicans belongs to the kingdom Fungi, under the phylum Ascomycota, class Saccharomycetes, order Saccharomycetales, family Saccharomycetaceae, and genus Candida. It was first described in the 19th century and is the most prevalent species within the genus linked to human infections.
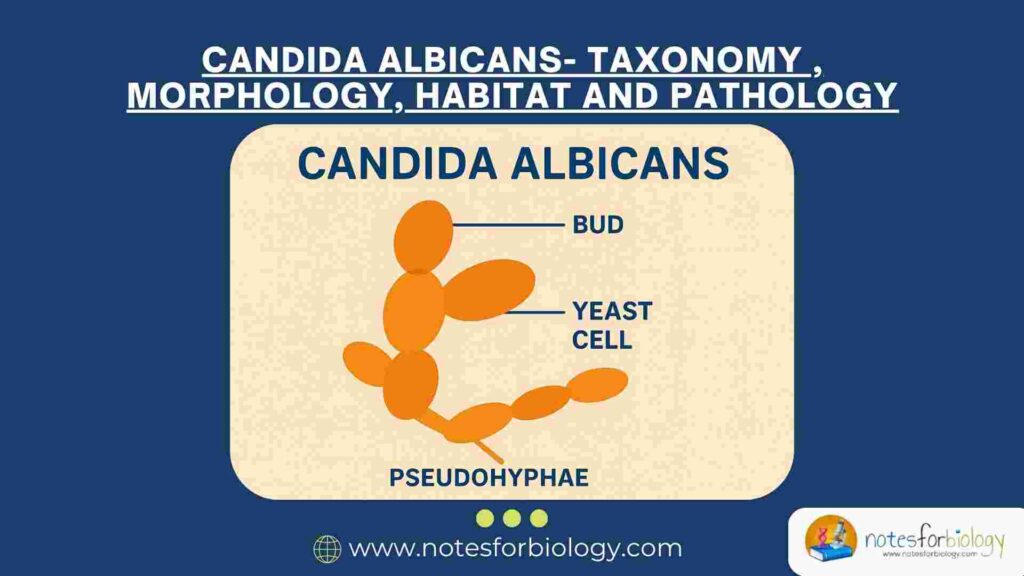
Yeast Form
In its yeast form, C. albicans exists as unicellular, oval-shaped cells that reproduce by budding. This form is typically found colonizing healthy mucosal surfaces and is regarded as the commensal or non-pathogenic state. Yeast cells are about 3–6 micrometers in diameter and can be observed in clinical samples as individual or budding cells under the microscope.
Pseudohyphae and True Hyphae
A hallmark of Candida albicans’ virulence is its polymorphic nature, enabling it to switch between yeast and filamentous forms. Pseudohyphae are chains of elongated, oval cells joined end-to-end with constrictions between cells, resembling elongated buds. True hyphae are longer, tubular, and have parallel sides without constrictions. Both filamentous forms are more invasive and associated with tissue penetration and biofilm formation.
The ability to transition between these forms is regulated by environmental cues such as temperature, pH, nutrient availability, and host immune signals. This morphological plasticity aids in evading host defenses and colonizing different niches.
Habitat and Normal Flora
Candida albicans is a commensal organism, meaning it naturally inhabits the human body without causing disease in healthy individuals. It mainly colonizes moist mucosal surfaces where it coexists with other microbial flora.
Oral Cavity
In the mouth, Candida albicans is found on the tongue, buccal mucosa, and dental surfaces. Its growth is normally controlled by saliva, competing bacteria, and the local immune system.
Gastrointestinal Tract
C. albicans colonizes the esophagus, stomach, and intestines as part of the gut flora. It plays a role in the complex microbiome but is kept in check by bacterial populations and immune surveillance.
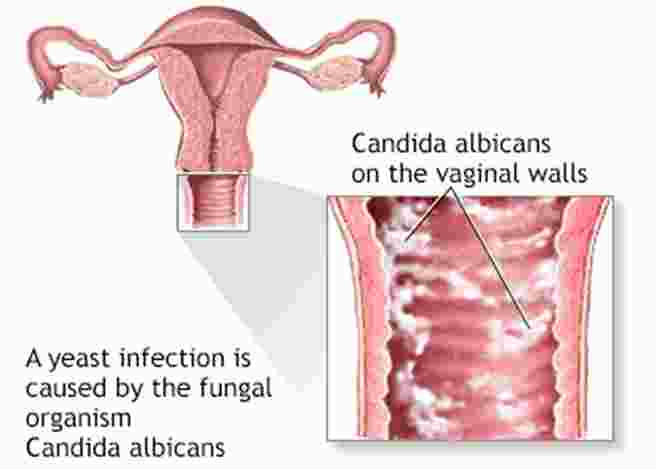
Genitourinary Tract
The vaginal mucosa is another common site of colonization. Under normal acidic pH and balanced bacterial flora, Candida albicans remains harmless. Disruption of this balance, for example, by antibiotics or hormonal changes, can lead to overgrowth and infection.
Skin and Nails
Although less common, C. albicans can also be found on skin surfaces and around nails, especially in moist areas. Here, it usually exists in low numbers without causing symptoms.
The maintenance of Candida albicans as part of the normal flora depends on a delicate equilibrium with host factors and other microorganisms. When this balance is disturbed, the yeast can become pathogenic.
Pathogenicity and Virulence Factors
Candida albicans’ ability to cause disease depends on various virulence factors that enable colonization, invasion, immune evasion, and damage to host tissues.
Adhesion to Host Cells
The initial step in infection is adhesion. C. albicans expresses surface proteins known as adhesins, which mediate attachment to epithelial and endothelial cells. These adhesins recognize specific host cell receptors, allowing the fungus to firmly attach and resist mechanical clearance.
Adhesion is critical for colonization and biofilm formation on tissues and medical devices such as catheters.
Morphological Plasticity
The yeast-to-hyphae transition is a key virulence trait. Filamentous forms penetrate tissues more efficiently and induce damage. Hyphae can also trigger host cell endocytosis, facilitating fungal invasion.
This morphological switch is regulated by complex signaling pathways responsive to environmental conditions, allowing adaptation and survival.
Secretion of Hydrolytic Enzymes
Candida albicans produces a range of secreted enzymes that facilitate tissue invasion and nutrient acquisition. Aspartyl proteases degrade host proteins including extracellular matrix components and immune factors. Phospholipases hydrolyze phospholipids in host cell membranes, promoting cell damage. Lipases break down lipids for fungal metabolism.
These enzymes help the fungus invade deeper tissues and evade immune defenses.
Biofilm Formation
Biofilms are structured communities of fungal cells embedded in an extracellular matrix. C. albicans forms biofilms on mucosal surfaces and implanted medical devices, which are highly resistant to antifungal agents and immune attack.
Biofilms contribute to persistent infections and increase the difficulty of eradication.
Phenotypic Switching
C. albicans can undergo reversible phenotypic switching between different colony morphologies (white, opaque, and others). This switching alters virulence attributes, mating competence, and immune recognition, enabling adaptation to various host niches.
Clinical Manifestations
The spectrum of diseases caused by Candida albicans is broad, reflecting its ability to infect superficial and deep tissues.
Superficial Candidiasis
Superficial infections are common and involve mucosal surfaces and skin.
Oral Candidiasis (Thrush): Characterized by creamy white plaques on the tongue and oral mucosa, which can be wiped off leaving an erythematous base. It is common in infants, elderly, and immunocompromised individuals.

Vulvovaginal Candidiasis: Presents with itching, burning, white discharge, and inflammation of the vaginal mucosa. It often occurs after antibiotic use, pregnancy, or diabetes.
Cutaneous Candidiasis: Infection of moist skin folds such as the groin, axilla, and under breasts presents with red, moist, macerated lesions that may be itchy or painful.

Chronic Mucocutaneous Candidiasis
A rare condition involving persistent and recurrent Candida infections of the skin, nails, and mucous membranes, usually due to genetic or acquired immune defects.
Invasive Candidiasis
When the fungus invades the bloodstream or internal organs, it causes candidemia and disseminated candidiasis, which are life-threatening.
Risk Factors: Include immunosuppression (HIV, chemotherapy), prolonged antibiotic use, central venous catheters, intensive care unit stay, and major surgery.
Clinical Presentation: Fever unresponsive to antibiotics, septic shock, organ dysfunction.
Organ Involvement: Kidneys, liver, spleen, heart valves (endocarditis), eyes (endophthalmitis), and central nervous system.
Diagnosis
Diagnosis of Candida albicans infection relies on a combination of clinical suspicion and laboratory techniques.
Direct Microscopic Examination
Scrapings or fluid samples are examined microscopically after treatment with KOH or Calcofluor White stain. The presence of budding yeast cells, pseudohyphae, or true hyphae supports Candida infection.
Culture
Samples are cultured on Sabouraud dextrose agar or chromogenic media. Colonies of C. albicans typically appear creamy, smooth, and may produce a distinctive green color on chromogenic agar.
Germ Tube Test
C. albicans produces germ tubes (short hyphal outgrowths) when incubated in serum at 37°C for 2–3 hours. This test is a rapid presumptive identification method.
Serological and Molecular Methods
Antigen detection tests, PCR assays, and DNA sequencing can confirm species and detect invasive candidiasis earlier than culture.
Histopathology
Tissue biopsy stained with periodic acid-Schiff (PAS) or Gomori methenamine silver (GMS) can reveal fungal invasion.
Treatment
Treatment strategies depend on infection severity, site, and patient risk factors.
Topical Antifungals
Mild superficial infections are managed with topical antifungal creams, ointments, or mouth rinses containing clotrimazole, nystatin, miconazole, or ketoconazole.
Systemic Antifungals
Invasive or recurrent infections require systemic therapy. Fluconazole is commonly used for mucosal infections and candidemia. Echinocandins (caspofungin, micafungin) are preferred for critically ill patients or fluconazole-resistant infections.
Amphotericin B is reserved for severe or refractory cases.
Removal of Predisposing Factors
Where possible, eliminating or managing predisposing factors such as indwelling catheters, broad-spectrum antibiotics, or immunosuppressive drugs is important for successful treatment.
Antifungal Resistance in Candida albicans
The rise of antifungal resistance in Candida albicans has become a critical concern in clinical treatment, as it reduces the effectiveness of commonly used antifungal drugs and complicates patient management.
Mechanisms of Resistance
Candida albicans employs several mechanisms to survive antifungal drug exposure. One common mechanism is mutations in the genes encoding the target enzymes of antifungal drugs. For example, mutations in the ERG11 gene, which encodes the enzyme lanosterol 14-α-demethylase, reduce the binding affinity of azole drugs such as fluconazole, leading to resistance.
Another important mechanism is the overexpression of efflux pumps. These are transporter proteins that actively expel antifungal drugs from the fungal cell, lowering intracellular drug concentrations and allowing the fungus to survive otherwise inhibitory drug levels.
Biofilms formed by Candida albicans also contribute to resistance. The dense extracellular matrix and altered metabolic state within biofilms hinder antifungal penetration and reduce drug efficacy, making infections involving biofilms especially difficult to eradicate.
Clinical Implications
The emergence of resistant Candida albicans strains necessitates careful antifungal susceptibility testing to guide effective therapy. Resistance often results in treatment failure, prolonged infection, and increased mortality, particularly in immunocompromised or critically ill patients.
Prevention of Candida albicans Infections
Preventing Candida albicans infections involves strategies aimed at maintaining the natural balance of microbial flora and minimizing exposure to risk factors that favor fungal overgrowth.
Maintaining Healthy Microbial Flora
Good personal hygiene, including regular oral care and skin cleanliness, helps prevent Candida colonization from progressing to infection. Avoiding unnecessary antibiotic use preserves the natural bacterial flora that competitively inhibits Candida growth on mucosal surfaces.
Management of Predisposing Factors
Patients with chronic illnesses such as diabetes, or those receiving immunosuppressive therapies, should be carefully monitored and managed to reduce susceptibility. Proper care and timely removal of indwelling medical devices like catheters decrease the risk of biofilm-associated infections.
Prophylactic Antifungal Use
In high-risk groups—such as patients undergoing chemotherapy or organ transplantation—prophylactic antifungal medications may be employed to prevent candidiasis. However, this approach requires balancing benefits with the risk of promoting antifungal resistance.
Conclusion
Candida albicans is a ubiquitous fungal species that balances its existence between commensalism and pathogenicity. Its ability to change morphology, adhere to host tissues, produce enzymes, and form biofilms contributes to its success as a pathogen. Clinical manifestations vary widely, necessitating accurate diagnosis and tailored treatment.
While generally manageable, invasive candidiasis remains a serious threat, particularly in immunocompromised individuals. Understanding Candida albicans biology and clinical impact is crucial for effective management and prevention of these infections.
Frequently Asked Questions (FAQ)
What is Candida albicans caused by?
It’s caused by an overgrowth of the fungus Candida albicans, usually when immunity is weak or the normal microbial balance is disturbed.
What is the best treatment for Candida albicans?
Topical antifungals for mild cases and oral or IV antifungals like fluconazole or echinocandins for severe or systemic infections.
What does it mean when Candida albicans is positive?
It means Candida albicans was detected in a sample, indicating colonization or an active fungal infection depending on symptoms and site.
Related Contents
Campylobacter Blood Agar (CVA)- Composition, Principle, Preparation, Results, Uses
Calcofluor White Staining- Principle, Procedure, Results, Applications