Campylobacteriosis is a common bacterial infection that causes food poisoning. It’s mostly caused by bacteria from the genus Campylobacter, especially Campylobacter jejuni. These bacteria are one of the leading causes of gastroenteritis (inflammation of the stomach and intestines) worldwide. Though it often results in mild illness, it can sometimes lead to serious complications, especially in children, the elderly, and people with weak immune systems.
What is Campylobacter?
Campylobacter is a type of bacteria that lives in the intestines of animals, especially birds. It is spiral-shaped, motile (can move), and microaerophilic, meaning it needs very little oxygen to grow. The most common species that cause infection in humans are:

- Campylobacter jejuni
- Campylobacter coli
These bacteria are sensitive to heat and proper cooking kills them. But they are surprisingly good at surviving in undercooked meat, raw milk, and contaminated water.
Summary of Campylobacteriosis
- Campylobacteriosis is an infection caused by Campylobacter bacteria, typically spread through contaminated food or water.
- It mainly results in gastrointestinal issues like diarrhea, abdominal cramps, and fever.
- Although usually self-limiting, in rare cases it can lead to complications such as Guillain-Barré syndrome, reactive arthritis, or bacteremia.
Table of Contents
How Do You Get Infected? (Mode of Transmission)
Campylobacteriosis spreads mainly through the consumption of contaminated food or water. Common sources include:
- Undercooked chicken or meat
- Raw or unpasteurized milk
- Contaminated water (e.g., from lakes, rivers, or untreated supplies)
- Poorly washed fruits and vegetables
- Contact with infected animals (especially poultry, dogs, and cats)
- Cross-contamination in the kitchen (like using the same cutting board for raw chicken and vegetables)
The bacteria are present in animal feces, and even a small amount can cause illness — in fact, it takes fewer than 500 bacteria to make someone sick.
Who is at Risk?
Anyone can get Campylobacteriosis, but some people are more likely to experience severe illness:
- Young children under 5
- Older adults
- People with weakened immune systems
- Pregnant women
Also, people who frequently handle raw meat, such as butchers or food service workers, are at higher risk.
Pathogenesis: What Happens Inside the Body?
When Campylobacter enters the digestive tract, it attaches to the lining of the small intestine and releases toxins. These toxins damage the intestinal cells, triggering an inflammatory response. This leads to symptoms such as diarrhea, abdominal cramps, and fever.
The bacteria do not usually invade deeper tissues, but in some cases, especially in immunocompromised individuals, they may enter the bloodstream and cause more severe infections.
Symptoms of Campylobacteriosis Campylobacter Infection
Symptoms usually appear 2 to 5 days after exposure and may include:
- Diarrhea (often bloody)
- Abdominal cramps
- Fever
- Nausea and vomiting
- Malaise (general feeling of being unwell)
- Headache
Symptoms typically last about one week, but can linger longer in some individuals.
Complications (in Rare Cases)of Campylobacteriosis
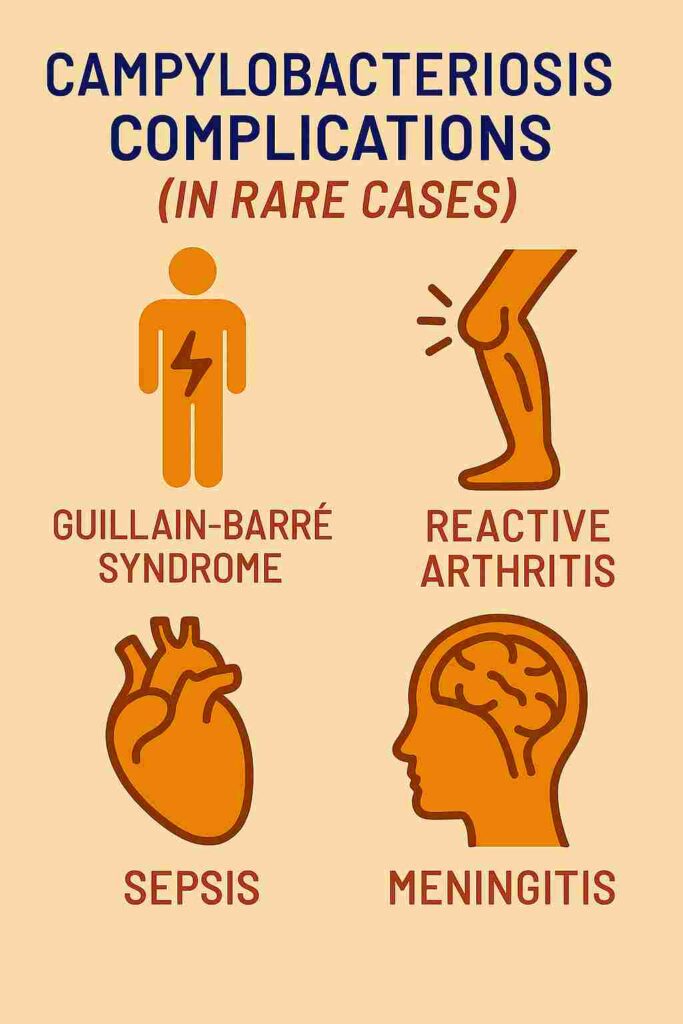
Though most cases are mild and self-limiting, complications can occur, such as:
- Guillain-Barré Syndrome (GBS): A rare but serious condition where the body’s immune system attacks the nerves. It can cause temporary paralysis.
- Reactive arthritis: Joint pain and swelling that can develop after infection.
- Sepsis: Blood infection, especially in people with weak immunity.
- Irritable bowel syndrome (IBS): Some individuals may develop long-term digestive issues.
- Meningitis: It is the inflammation of the protective membranes (meninges) surrounding the brain and spinal cord. It’s most often caused by an infection—either viral or bacterial—with the bacterial form generally being more severe and life-threatening. Common symptoms include fever, headache, neck stiffness, and sometimes sensitivity to light or confusion; in infants, signs might be irritability or poor feeding.
Diagnosis: How Is It Detected?
Diagnosis is usually based on clinical symptoms and confirmed by laboratory tests such as:
- Stool Culture: The most common method. A stool sample is taken and tested for the presence of Campylobacter bacteria.
- PCR (Polymerase Chain Reaction): A more sensitive test that detects bacterial DNA in the stool.
- Blood tests: Sometimes used to check for complications or rule out other causes.
Treatment of Campylobacteriosis
Most people recover without specific treatment. The main approach is supportive care, which includes:
- Hydration: Drink plenty of fluids to prevent dehydration. Oral rehydration salts (ORS) may be needed.
- Rest: Let your body fight off the infection naturally.
In severe cases, or when complications arise, doctors may prescribe antibiotics, such as:
- Azithromycin or Erythromycin
- Ciprofloxacin (though resistance is increasing)
Important: Antibiotics are not needed in most mild cases and should only be used under medical advice.
Prevention and Control
You can significantly reduce the risk of Campylobacter infection by following these steps:
1. Cook Thoroughly
- Cook all meat, especially chicken, to a safe internal temperature (at least 165°F or 75°C).
- Avoid eating raw or undercooked poultry.
2. Avoid Cross-Contamination
- Use separate cutting boards and utensils for raw meat and other foods.
- Wash hands, knives, and surfaces with soap and hot water after handling raw meat.
3. Drink Safe Water
- Drink boiled, treated, or bottled water when in doubt.
- Avoid swallowing water from lakes, rivers, or pools.
4. Avoid Raw Milk
- Drink only pasteurized milk and dairy products.
5. Practice Good Hygiene
- Wash hands before eating or preparing food.
- Wash hands after handling pets, cleaning up after animals, or using the toilet.
Global Impact and Epidemiology
- Campylobacteriosis is one of the most reported bacterial foodborne illnesses globally.
- According to WHO, it affects more than 550 million people every year, including 220 million children.
- The infection is more common in developing countries due to limited access to clean water and safe food handling.
- In high-income countries, most cases occur as sporadic infections, often linked to undercooked poultry or contaminated water.
Ongoing Research and Concerns
There is growing concern about antibiotic-resistant strains of Campylobacter. Overuse of antibiotics in animal farming is a major contributor. Research is ongoing to:
- Develop more effective diagnostic tools
- Monitor resistance patterns
- Create better food safety policies
- Investigate vaccine development (though none are currently approved for humans)
Conclusion
Campylobacteriosis is a common but often overlooked cause of food poisoning. While most cases are mild and resolve without treatment, the infection can be severe and lead to serious complications in vulnerable individuals. Good hygiene, safe food practices, and public awareness are key to preventing the spread of this disease. As antibiotic resistance rises, it’s more important than ever to be cautious with food handling and to follow public health guidelines.
With proper care and preventive measures, Campylobacter infections can be effectively controlled keeping our meals safe and our communities healthier.
Frequently Asked Questions (FAQs)
What is Campylobacteriosis?
Campylobacteriosis is an infection caused by the Campylobacter bacteria, primarily Campylobacter jejuni. It is one of the most common causes of bacterial gastroenteritis worldwide.
How do people get Campylobacter infection?
The primary mode of transmission is the consumption of contaminated food, especially undercooked poultry. Other sources include unpasteurized milk, untreated water, and contact with infected animals.
What is the treatment for Campylobacter infection?
Most cases are self-limiting and require supportive care, including hydration. In severe cases or for high-risk individuals, antibiotics such as azithromycin may be prescribed.
Related Articles