What is Histoplasma capsulatum?
Histoplasma capsulatum is a fascinating fungus that can switch between two forms depending on its environment. In nature, particularly in soil enriched with bird or bat droppings, it exists as a mold that releases tiny spores into the air. When people accidentally inhale these spores, the warmth of the human body triggers the fungus to transform into its yeast form, which can then cause an infection called histoplasmosis.
This disease is especially common in areas like the Ohio and Mississippi River valleys in the United States, where the fungus thrives in the soil. Activities that disturb contaminated soil such as farming, construction, or exploring caves increase the risk of inhaling the spores. While many healthy people may experience mild or no symptoms, those with weakened immune systems can develop serious lung infections or even systemic illness. To reduce the risk, it’s wise to take precautions like wearing masks in areas where the fungus is likely to be found, such as near bird roosts or bat habitats.
What is Histoplasmosis?

Histoplasmosis is the disease caused when humans inhale spores of this fungus, leading to infection (ranging from mild flu-like illness to severe lung/systemic disease).
Summary of Histoplasmosis
- Histoplasmosis is a lung infection caused by breathing in spores from soil contaminated with bird/bat droppings – common in certain U.S. regions.
- While many people get mild flu-like symptoms (or none), it can turn serious for those with weak immune systems, spreading beyond the lungs.
- Prevention is smart: mask up in dusty areas with droppings, and see a doctor if you develop cough/fever after exposure
Table of Contents
Types of Histoplasmosis
Histoplasmosis, caused by the fungus Histoplasma capsulatum, presents in various forms depending on the extent of infection and the individual’s immune status. Here’s an expanded overview of its types:
1. Acute Pulmonary Histoplasmosis
This is the most common form, often resulting from inhaling a small number of spores. Many individuals remain asymptomatic or experience mild flu-like symptoms such as fever, cough, chest pain, and fatigue. In cases of higher exposure, symptoms can resemble pneumonia, including shortness of breath and chest discomfort. Most healthy individuals recover without treatment, but symptoms can persist for weeks or months in some cases.
2. Chronic Cavitary Pulmonary Histoplasmosis
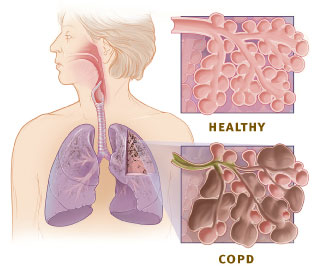
This form typically affects individuals with pre-existing lung conditions like emphysema or chronic obstructive pulmonary disease (COPD). Symptoms resemble those of tuberculosis and include a persistent cough, weight loss, night sweats, and fatigue. The infection can cause cavities in the lungs and may lead to progressive lung damage if left untreated. Long-term antifungal therapy is often required for management.
3. Progressive Disseminated Histoplasmosis
This severe form occurs when the infection spreads beyond the lungs to other organs, such as the liver, spleen, bone marrow, and central nervous system. It is more prevalent in immunocompromised individuals, including those with HIV/AIDS or undergoing chemotherapy. Symptoms can include fever, weight loss, fatigue, and organ-specific manifestations. Without prompt antifungal treatment, this form can be life-threatening.
4. Central Nervous System (CNS) Histoplasmosis
A rare but serious manifestation, CNS histoplasmosis occurs when the fungus infects the brain and spinal cord. It is often associated with disseminated disease and presents with neurological symptoms such as headaches, confusion, seizures, and neck stiffness. Diagnosis can be challenging, and treatment typically involves prolonged antifungal therapy.
Understanding the various forms of histoplasmosis is crucial for timely diagnosis and appropriate treatment, especially in individuals with weakened immune systems.
Pathogenesis of Histoplasmosis
The pathogenesis of histoplasmosis involves the inhalation of Histoplasma capsulatum spores, leading to a complex interaction between the fungus and the host’s immune system. Here’s a detailed overview:
1. Inhalation and Initial Infection
Histoplasma capsulatum is a dimorphic fungus found in soil enriched with bird or bat droppings. When this contaminated soil is disturbed, microscopic spores (microconidia) become airborne and can be inhaled into the lungs. Upon reaching the warm environment of the alveoli, these spores convert into their yeast form, which is pathogenic in humans.
2. Immune Response and Intracellular Survival
The yeast forms are quickly engulfed by alveolar macrophages, a type of immune cell in the lungs. However, H. capsulatum has evolved mechanisms to survive and replicate within these macrophages, effectively evading the host’s initial immune defenses. This intracellular survival allows the fungus to persist and multiply within the host.
3. Dissemination
In individuals with a healthy immune system, the infection is often contained within the lungs, and the person may remain asymptomatic or experience mild respiratory symptoms. However, in immunocompromised individuals, such as those with HIV/AIDS or undergoing immunosuppressive therapy, the fungus can disseminate from the lungs to other parts of the body, including the liver, spleen, bone marrow, and central nervous system. This widespread infection can lead to severe, life-threatening complications.
4. Granuloma Formation and Latency
The body’s immune response may lead to the formation of granulomas, which are clusters of immune cells that attempt to wall off the infection. These granulomas can calcify over time, effectively containing the fungus. However, the organism can remain dormant within these granulomas and may reactivate if the individual’s immune system becomes compromised in the future.
Understanding the pathogenesis of histoplasmosis is crucial for early diagnosis and effective treatment, especially in populations at higher risk for severe disease.
Laboratory Diagnosis of Histoplasmosis
Histoplasmosis can be diagnosed through various lab tests, each with its own strengths depending on the type and stage of infection. Here are the main diagnostic methods:
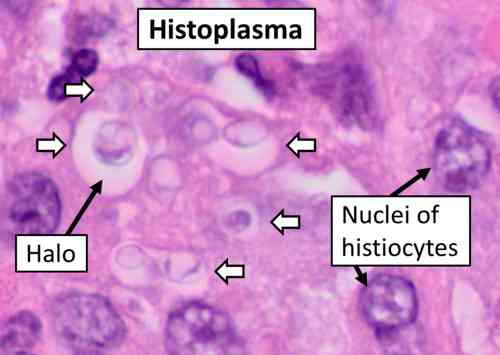
1. Microscopic Examination
This is the fastest way to detect Histoplasma in clinical samples. Stains like Giemsa or Wright can reveal tiny yeast cells (2–4 µm) in blood, bone marrow, or tissue. Special fungal stains (GMS or PAS) are used on tissue biopsies for clearer visualization.
2. Fungal Culture
Considered the most definitive test, but it takes time (2–6 weeks). Samples like blood, sputum, or tissue are cultured. The fungus grows as a mold at room temperature but switches to yeast form at body temperature (37°C).
3. Antigen Testing
A rapid and highly sensitive method, especially for disseminated histoplasmosis. The test detects Histoplasma antigens in:
- Urine (most common)
- Serum (blood)
- Cerebrospinal fluid (CSF) (if CNS involvement is suspected)
It’s useful for early diagnosis and monitoring treatment response.
4. Antibody Testing (Serology)
This detects the body’s immune response to the fungus. Two main tests are used:
- Complement Fixation (CF) – More sensitive but can cross-react with other fungi.
- Immunodiffusion (ID) – More specific but may miss early infections.
Best for chronic or pulmonary cases, but often negative in immunocompromised patients.
5. Molecular Testing (PCR)
A fast but still emerging method. PCR can detect Histoplasma DNA in blood, tissue, or respiratory samples. Not yet widely available but useful in specialized labs.
6. Histopathology (Tissue Biopsy)
If a tissue sample (e.g., lymph node, lung) is taken, pathologists look for granulomas with yeast-filled macrophages. Special stains (GMS, PAS) help confirm the diagnosis.
Which Test to Use?
- Acute pulmonary cases → Antigen test + serology
- Disseminated disease → Urine antigen + blood culture
- Chronic infections → Serology + sputum culture
- Immunocompromised patients → Antigen tests (since antibody responses may be weak)
Treatment of Histoplasmosis
The treatment of histoplasmosis depends on the severity of the disease and the patient’s immune status. Here’s an overview of the current management strategies:
1. Asymptomatic or Mild Cases
In immunocompetent individuals with asymptomatic or mild acute pulmonary histoplasmosis, antifungal therapy is often not required. These cases typically resolve without treatment. However, if symptoms persist beyond a month or worsen, antifungal treatment may be considered.
2. Moderate to Severe Acute Pulmonary Histoplasmosis
Patients exhibiting more pronounced symptoms may benefit from antifungal therapy. Itraconazole is commonly prescribed for these cases. In severe instances, initial treatment with liposomal amphotericin B is recommended, followed by a course of itraconazole once the patient stabilizes.
3. Chronic Pulmonary Histoplasmosis
This form resembles tuberculosis and requires prolonged antifungal treatment. Itraconazole is the drug of choice, typically administered for 12 to 24 months.
4. Disseminated Histoplasmosis
In cases where the infection spreads beyond the lungs, especially in immunocompromised individuals, prompt antifungal therapy is crucial. Liposomal amphotericin B is used initially, followed by a maintenance regimen of itraconazole for at least 12 months.
5. Central Nervous System (CNS) Histoplasmosis
For infections involving the CNS, liposomal amphotericin B is administered initially, followed by itraconazole. Alternative antifungals like voriconazole or posaconazole may be considered if itraconazole is not tolerated.
Monitoring and Considerations
Regular monitoring of drug levels and liver function tests is essential during treatment, especially with itraconazole, to ensure efficacy and minimize toxicity. Adjustments may be necessary based on patient response and potential drug interactions.
It’s important to consult healthcare professionals for individualized treatment plans, as management may vary based on specific patient factors and emerging clinical guidelines.
Prevention and Control of Histoplasmosis
Since Histoplasma capsulatum thrives in soil contaminated with bird or bat droppings, prevention focuses on reducing exposure to fungal spores. Here are the key strategies:
1. Avoid High-Risk Environments
The most effective way to prevent histoplasmosis is to avoid areas where the fungus grows. This includes places with accumulated bird or bat droppings such as chicken coops, old barns, caves, and attics. The fungus is particularly common in the Ohio and Mississippi River valleys in the U.S. If you must enter these areas, take precautions like wetting the soil first to reduce dust, and consider hiring professionals for large clean-up jobs. Activities that disturb soil like digging, construction, or demolition in endemic areas should be approached with caution.
2. Personal Protection
When exposure is unavoidable, proper protective equipment is essential:
- Wear N95 respirators to filter out fungal spores
- Use gloves, long sleeves, and boots when handling contaminated materials
- Practice good hygiene by showering and changing clothes after potential exposure
3. Environmental Control
Proper cleaning and maintenance can reduce risks:
- Decontaminate areas with bird/bat droppings using a 10% bleach solution
- Keep work areas well-ventilated
- Maintain landscaping to prevent organic material buildup
- Consider professional remediation for heavily contaminated sites
4. Special Precautions for High-Risk Groups
Immunocompromised individuals need extra protection:
- HIV/AIDS patients and transplant recipients should avoid high-risk activities
- Workers in endemic areas should follow OSHA safety guidelines
- Employers should provide proper training about histoplasmosis risks
5. Early Detection and Treatment
Be alert for symptoms after potential exposure:
- Common signs include fever, cough and fatigue
- Diagnostic tests like urine antigen tests can provide rapid results
- Treatment with antifungals (itraconazole, amphotericin B) is effective when started early
Prevention through avoidance of contaminated areas and proper protective measures is the best defense against histoplasmosis. Early diagnosis and treatment are crucial for those who develop symptoms after exposure.
Conclusion
In conclusion, histoplasmosis is a fungal infection caused by Histoplasma capsulatum, commonly found in environments with bird or bat droppings. While many individuals may experience mild or no symptoms, the disease can become severe, especially in immunocompromised persons. Timely diagnosis and appropriate treatment are crucial to prevent complications.
Preventive measures, such as avoiding exposure to contaminated environments and using protective equipment, are essential, particularly for those at higher risk. Awareness and early intervention remain key to managing and controlling histoplasmosis effectively.
Frequently Asked Questions (FAQs)
What is Histoplasmosis?
Histoplasmosis is a fungal infection caused by inhaling spores of Histoplasma capsulatum, commonly found in environments contaminated with bird or bat droppings. It primarily affects the lungs but can spread to other organs, especially in individuals with weakened immune systems.
How is Histoplasmosis contracted?
People become infected by breathing in microscopic fungal spores present in the air, often after disturbing contaminated soil during activities like construction, excavation, or exploring caves.
What are the symptoms of Histoplasmosis?
Symptoms vary depending on the severity of the infection. Mild cases may be asymptomatic or present flu-like symptoms, while severe cases can cause chronic cough, chest pain, fever, fatigue, and in disseminated forms, affect multiple organs leading to serious health complications.
Related Articles