T cells, or T lymphocytes, are a critical component of the adaptive immune system. Their roles include identifying and eliminating pathogens and cancer cells, as well as orchestrating other aspects of the immune response. The journey of T cells from their origins to their final, mature functional states involves complex processes of maturation, activation, and differentiation. Here, we delve into these stages in detail.
Table of Contents
T-cell maturation
T-cell maturation is the process by which precursor T cells (thymocytes) evolve into mature, functioning T cells that can participate in the adaptive immune response. This maturation takes place predominantly in the thymus, which is located in the chest. The process has numerous stages, including the formation and selection of T cells capable of recognizing antigens presented by self-MHC (Major Histocompatibility Complex) molecules, as well as the elimination of T cells that are extremely self-reactive in order to prevent autoimmunity.
Key stages of T-cell maturation
Migration to the thymus
T-cell progenitors arise in the bone marrow and move to the thymus to mature.
Thymic Architecture:
The thymus is separated into two parts: the cortex and the medulla, which perform unique roles in T-cell development.
Double Negative Stage (DN):
Thymocytes in their early stages do not express CD4 or CD8 co-receptors (thus the term “double negative”).
These cells go through numerous rounds of proliferation and gene rearrangement for the T-cell receptor (TCR).
TCR gene rearrangement:
β-Chain Rearrangement: TCR β-chain genes rearrange first. Successful rearrangement results in the expression of a pre-TCR complex.
α-Chain Rearrangement: After successful β-chain expression, the α-chain genes rearrange to form a functioning TCR.
Double-positive stage (DP):
Thymocytes exhibit both CD4 and CD8 co-receptors (“double positive”).
These cells go through positive and negative selection processes.
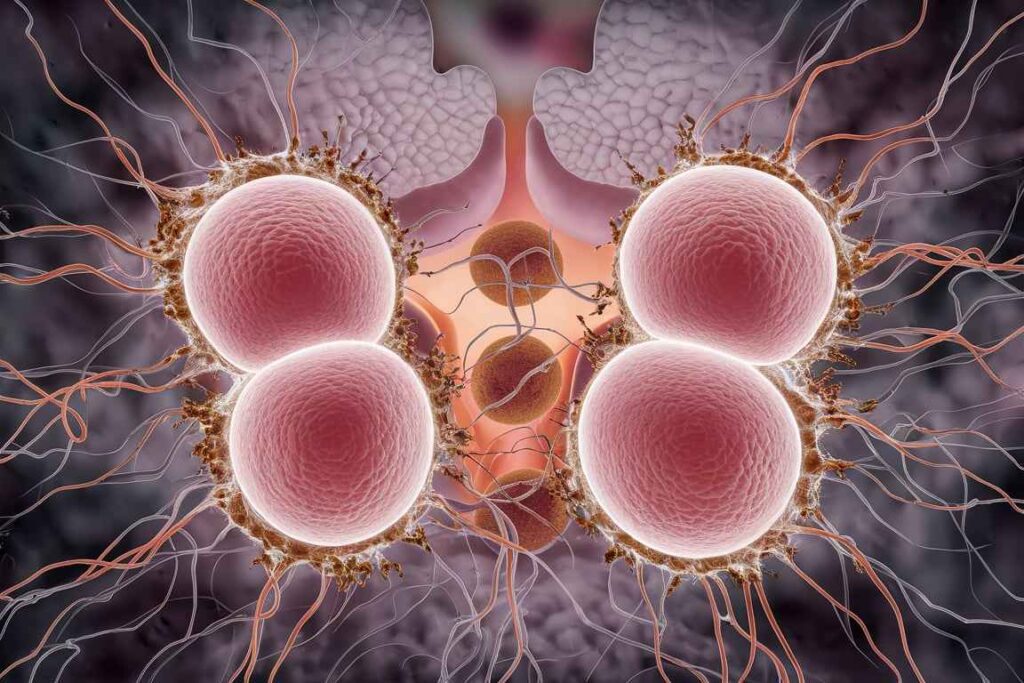
Positive selection:
Location: Thymic cortex.
Thymocytes must detect and bind to self-MHC molecules expressed by cortical thymic epithelial cells (cTECs). Thymocytes with a moderate ability to bind to self-MHC molecules receive survival signals.
Thymocytes that are unable to bind to their own MHC molecules die.
Lineage Commitment:
Thymocytes that successfully undergo positive selection commit to either the CD4+ or CD8+ lineage depending on their interaction with MHC molecules:
CD4+ T cells bind to MHC class II molecules.
CD8+ T cells bind to MHC class I molecules.
Negative Selection:
Location: In the thymic medulla.
Thymocytes attach tightly to self-antigens provided by medullary thymic epithelial cells (mTECs) and dendritic cells undergo apoptosis.
Outcome: This process eliminates self-reactive T cells, preventing autoimmunity. This is a crucial step in establishing central tolerance.
Single Positive Stage (SP):
Thymocytes become either CD4+ or CD8+ single-positive T cells, depending on their interactions during positive selection.
Final Maturation:
Mature single-positive T cells exit the thymus and enter the peripheral circulation as naïve T cells. These cells are now capable of recognizing antigens presented by self-MHC molecules and can participate in immune responses
Molecular and cellular players
Thymic epithelial cells (TECs)
Cortical TECs (cTECs) are involved in positive selection.
Medullary TECs (mTECs) are involved in negative selection and the presentation of self-antigens.
Dendritic cells and macrophages
Present self-antigens in the thymus to facilitate negative selection.
Cytokine and Growth Factors:
Several cytokines, including interleukins and thymic stromal lymphopoietin, promote T-cell growth and proliferation.
Transcription Factors
T-bet, GATA-3, RORγt, and Foxp3 help differentiate T cells into functional subsets (Th1, Th2, Th17, Treg).
Importance of T-cell maturation
T-cell maturation is required for the formation of a functioning, self-tolerant T-cell repertoire. This procedure guarantees that:
- Self-MHC Restriction: T lymphocytes detect antigens provided by self-MHC molecules, which is necessary for efficient antigen presentation.
- Central tolerance involves the elimination of self-reactive T cells, which prevents autoimmune reactions.
- varied Repertoire: The immune system generates a varied set of TCRs, allowing it to recognize a wide range of antigens.
Frequently Asked Question
What T-cell maturation ?
T-cell maturation is the process by which precursor T cells (thymocytes) evolve into mature, functioning T cells that can participate in the adaptive immune response. This maturation takes place predominantly in the thymus, which is located in the chest.
What are the importance of T-cell maturation?
The importance of T-cell maturation are
1. Self-MHC Restriction
2. Central tolerance
3. varied Repertoire
Related Article
Single cell protein (SCP): Substrate and steps involved in production