Mechanism of Respiration in Humans: Oxygen Absorption and Carbon Dioxide Release
The mechanism of respiration in humans is all about how we take in oxygen and get rid of carbon dioxide. This process is essential for our bodies because it allows us to absorb oxygen (O₂) and remove carbon dioxide (CO₂), which is a waste product from how our cells function. There are two main parts to this mechanism: external respiration, which involves breathing and gas exchange in the lungs, and internal respiration, which is about gas exchange at the tissue level. Together, these processes ensure that our bodies can effectively exchange and use the gases that are crucial for our cells to work properly, helping to keep everything balanced and supporting our overall health.
Table of Contents
1. External Respiration (Breathing and Gas Exchange in the Lungs)
External respiration encompasses the physical act of breathing as well as the gas exchange that occurs in the lungs. The mechanism of respiration in humans depends on the diaphragm and the intercostal muscles, which help enable inhalation and exhalation.
1.1 Anatomy of the Respiratory System
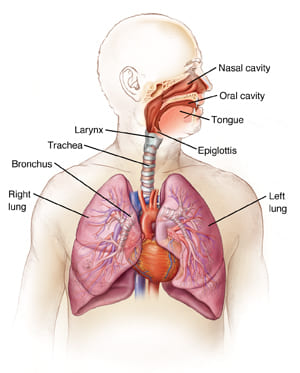
The respiratory system consists of several essential components that collaborate to facilitate air movement in and out of the lungs, where gas exchange occurs:
- Nasal Cavity: Air flows into the respiratory system via the nostrils and moves through the nasal cavity, where it is filtered, warmed, and humidified by mucus and cilia.
- Pharynx: This refers to the throat region that links the nasal and oral cavities to the larynx (voice box) and esophagus.
- Larynx (Voice Box): The larynx houses the vocal cords and acts as a conduit for air to travel from the pharynx to the trachea.
- Trachea (Windpipe): A sturdy conduit that links the larynx to the bronchi, facilitating air flow into the lungs.
- Bronchi and Bronchioles: The trachea splits into two main bronchi (one for every lung). These continue to split into smaller bronchioles that distribute air throughout the lungs.
- Lungs: The lungs serve as the primary organs for gas exchange, facilitating the absorption of oxygen into the blood and the release of carbon dioxide. The lungs have millions of small air sacs known as alveoli, where gas exchange takes place.
1.2 Mechanics of Breathing
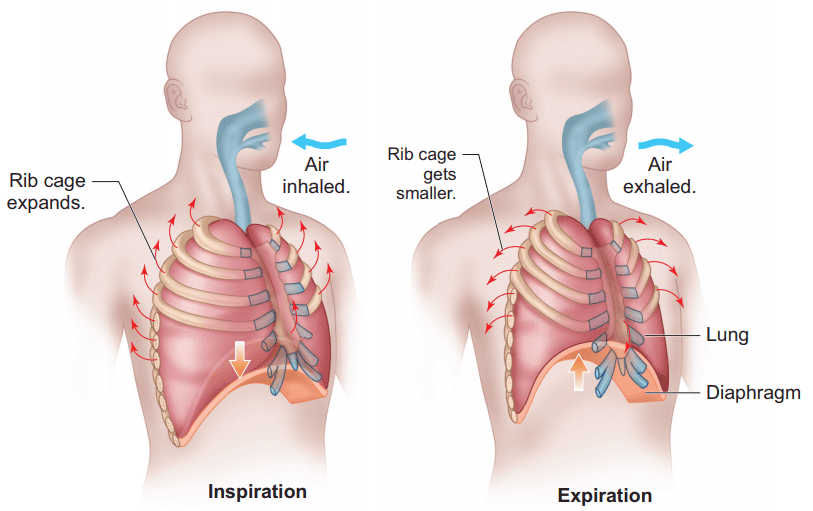
Breathing consists of two primary phases: inhalation (inspiration) and exhalation (expiration).
Inhalation (Inspiration)
- Muscle Function: When inhaling, the diaphragm (a major muscle situated below the lungs) contracts and descends. This enlarges the capacity of the thoracic (chest) cavity.
- Rib Motion: The external intercostal muscles (located between the ribs) contract, raising the ribs and further enlarging the chest cavity.
- Pressure Variation: When the volume of the chest cavity expands, the pressure within the lungs (intrapulmonary pressure) decreases below atmospheric pressure. This establishes a pressure difference that enables air to flow rapidly into the lungs.
- Airflow: Air enters the body via the nose or mouth, goes down the trachea, and flows into the lungs through the bronchi and bronchioles, ultimately arriving at the alveoli.
Exhalation (Expiration)
- Muscle Relaxation: Breathing out is usually a passive action. The diaphragm relaxes and shifts upward into the thoracic cavity, while the external intercostal muscles also relax, leading the rib cage to revert to its resting position.
- Pressure Variation: When the chest cavity reduces in size, the intrapulmonary pressure elevates above atmospheric pressure, resulting in air moving out of the lungs.
- Airflow: Air is released from the alveoli, moves upward through the bronchioles, bronchi, and trachea, and leaves via the mouth or nose.
2. Gas Exchange in the Alveoli
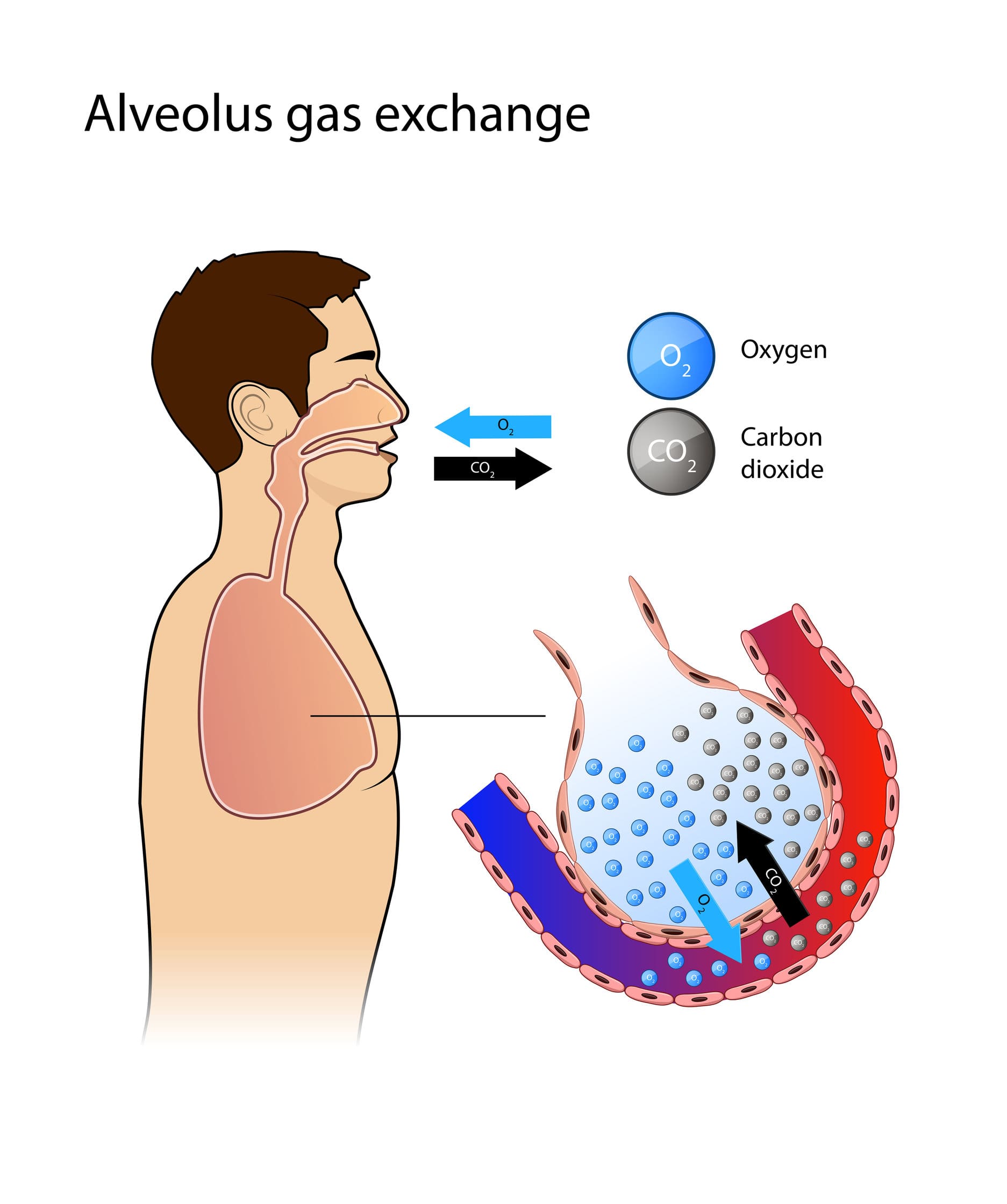
Gas exchange takes place in the alveoli, which are small, balloon-shaped formations in the lungs. The alveoli are encircled by a thick mesh of capillaries (tiny blood vessels) that facilitate the exchange of oxygen and carbon dioxide between the air and blood.
2.1 Structure of the Alveoli
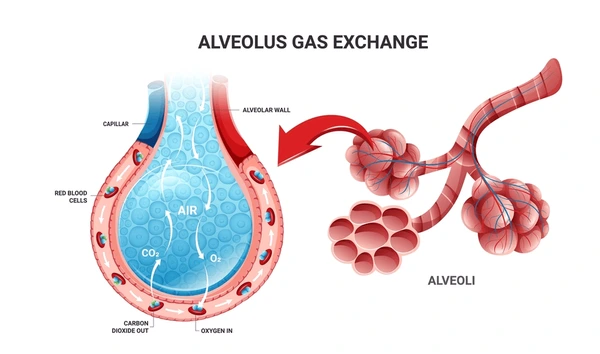
The alveoli are ideally structured for gas exchange due to their:
- Thin Walls: The walls of the alveoli consist of a single layer of epithelial cells, enabling gases to easily pass through.
- Extensive Surface Area: The alveoli possess an extensive surface area because of their many small sacs, enhancing the efficiency of gas exchange.
- Capillaries: A dense network of tiny blood vessels encircles the alveoli. The capillary walls are extremely thin as well, facilitating the easy diffusion of gases between the alveolar air and the blood.
2.2 Gas Exchange Process.
- Oxygen Transport: When air enters the alveoli, oxygen shifts from the alveolar air (where the partial pressure of oxygen is greater) into the blood (where the partial pressure of oxygen is lesser). The oxygen subsequently attaches to hemoglobin in red blood cells, creating oxyhemoglobin.
- Carbon Dioxide Removal: Carbon dioxide, a byproduct of cellular metabolism, transfers from the blood (where its partial pressure is elevated) into the alveoli, from which it will be exhaled.
2.3 Factors Affecting Gas Exchange
Numerous elements influence the efficiency of gas exchange:
- Concentration Gradient: The exchange of gases depends on variations in the partial pressures of oxygen and carbon dioxide within the alveoli and bloodstream. Oxygen travels from regions of high partial pressure (in the alveoli) to regions of lower partial pressure (in the blood), whereas carbon dioxide flows in the reverse direction.
- Surface Area: A larger surface area of the alveoli leads to more effective gas exchange.
- Thickness of the Respiratory Membrane: The more slender the membrane separating the alveolar air from the blood, the simpler it becomes for gases to diffuse.
3. Internal Respiration (Cellular Respiration and Gas Exchange at the Tissue Level)
Internal respiration involves the gas exchange at the cellular level, where oxygen is provided to cells, and carbon dioxide is removed.
3.1 Oxygen Transport to Tissues
After oxygen attaches to hemoglobin in red blood cells, it is transported via the bloodstream to various tissues in the body. In the tissues, hemoglobin releases oxygen (as the partial pressure of oxygen is reduced) and it diffuses into the cells, where it is utilized in cellular respiration to generate energy (ATP).
3.2 Carbon Dioxide Transport from Tissues
Carbon dioxide is generated during cellular metabolism and travels from the cells into the bloodstream as a key part of the mechanism of respiration. This process plays an essential role in keeping the gas levels in the body balanced. From there, carbon dioxide is transported back to the lungs using three primary methods, all of which are vital to the mechanism of respiration.
- As Bicarbonate Ions (HCO₃⁻): The majority of carbon dioxide (approximately 70%) is transported as bicarbonate ions in the bloodstream. The enzyme carbonic anhydrase facilitates the transformation of CO₂ and water into carbonic acid, which subsequently breaks down into bicarbonate and hydrogen ions.
- Bound to Hemoglobin: Approximately 20% of carbon dioxide attaches directly to hemoglobin, resulting in carbaminohemoglobin.
- Dissolved in Plasma: Approximately 10% of carbon dioxide is directly dissolved in the plasma.
3.3 Return of Carbon Dioxide to the Lungs
When carbon dioxide gets to the lungs, it moves from the blood into the alveoli, ready to be exhaled as part of the mechanism of respiration. The enzyme carbonic anhydrase helps with this by converting bicarbonate ions into CO₂, which is important for the overall function of the mechanism of respiration.
4. Regulation of Breathing
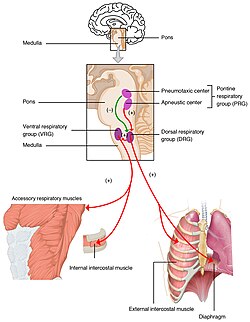
The mechanism of respiration is controlled by specific centers in the brainstem that keep an eye on the levels of oxygen, carbon dioxide, and pH in our blood. When these levels change, these centers adjust the mechanism of respiration by modifying how fast or deep we breathe, helping to maintain the right balance of gases in our bodies for overall health.
4.1 Respiratory Control Centers
The medulla oblongata and pons, located in the brainstem, are key players in controlling the mechanism of respiration and the entire breathing process. These areas are vital for making sure that the mechanism of respiration operates seamlessly and efficiently.
- Medulla: The medulla has two respiratory centers—the dorsal respiratory group (DRG) and the ventral respiratory group (VRG)—that regulate the fundamental rhythm and rate of respiration.
- Pons: The pons assists in managing the switch between inhaling and exhaling, and modifies the breathing rhythm during actions such as talking or exercising.
4.2 Chemoreceptors and Gas Levels
Chemoreceptors in the blood vessels (mainly in the carotid and aortic bodies) monitor the levels of oxygen, carbon dioxide, and pH in the blood. These receptors help regulate breathing:
- Central Chemoreceptors: Found in the medulla, these receptors detect changes in CO₂ levels (which affect blood pH). When CO₂ levels rise, the blood becomes more acidic, and the body increases the rate and depth of breathing.
- Peripheral Chemoreceptors: Located in the carotid and aortic bodies, these receptors detect oxygen levels in the blood. When oxygen levels drop, they signal the brain to increase breathing.
4.3 Other Factors Affecting Respiration
The mechanism of respiration is essential for our survival, as it enables our bodies to take in oxygen and remove carbon dioxide. When this process is disrupted, it can lead to health problems from insufficient oxygen and the buildup of waste gases. Being aware of the factors that can affect the mechanism of respiration is important for maintaining respiratory health. Here are some key elements that can influence it:
- Stretch Receptors: Found in the lungs, these receptors avert overinflation by sending signals to the brain to halt inhalation when the lungs reach full expansion (Hering-Breuer reflex).
- Voluntary Regulation: The cerebral cortex enables voluntary regulation of breathing, including activities like holding one’s breath or managing breath while speaking.
Conclusion
The mechanism of respiration in humans is essential for our survival, as it involves taking in oxygen and eliminating carbon dioxide, both of which are crucial for generating energy in our bodies. Our lungs facilitate this important gas exchange, while our brains regulate the process to ensure we receive enough oxygen. However, factors like air quality, physical activity, and existing health conditions can impact how effectively we breathe. This highlights the importance of maintaining a healthy lifestyle—engaging in regular exercise and steering clear of pollutants can significantly enhance our respiratory health. By being mindful of the mechanism of respiration, we can improve our overall well-being and enjoy a longer, healthier life.
Frequently Asked Questions (FAQ)
How does the mechanism of respiration work?
The mechanism of respiration consists of two primary phases: external respiration, which encompasses the act of breathing and gas exchange within the lungs, and internal respiration, which pertains to gas exchange occurring at the cellular level.
What are alveoli, and why are they important for gas exchange?
Alveoli are small, balloon-shaped structures within the lungs that facilitate gas exchange. Their walls are thin and encircled by a network of capillaries. Oxygen from the air we breathe moves through the alveolar walls into the blood, whereas carbon dioxide present in the blood travels into the alveoli to be expelled. Their extensive surface area and thin membrane render them very effective for gas exchange.
Discuss the impact of various respiratory disorders on the mechanism of respiration.
Respiratory conditions such as asthma and COPD disrupt the mechanism of respiration by constricting airways or harming alveoli. This results in decreased gas exchange and impacts the effectiveness of the mechanism of respiration
Related Articles