An eye infection is an inflammatory disorder caused by bacteria, viruses, fungus, or parasites that can produce redness, swelling, pain, discharge, and reduced vision, depending on the kind and degree of the infection.
Table of Contents
Eye Infections: Detailed Overview
Types of Eye Infection
- Conjunctivitis (Pink Eye)
- Keratitis
- Blepharitis
- Endophthalmitis
1. Conjunctivitis (pink eye)
Causative agents
Bacterial:
- Staphylococcus aureus.
- Streptococcus pneumoniae
- Haemophilus influenzae.
Viral:
- Adenoviruses
- Herpes Simplex Virus (HSV)
Allergies:
- Agents include pollen, dust mites, animal dander, and molds.
- Symptoms include itchy eyes, redness, runny discharge, and swollen eyelids. Seasonal or allergy-related.
- Diagnosis is based on a clinical examination and patient history. Allergy testing can help identify specific allergens.
2. Keratitis
Types and Causative Agents:
Bacterial keratitis:
- Agents include Pseudomonas aeruginosa (common among contact lens wearers), Staphylococcus aureus, and Streptococcus pneumoniae.
- Symptoms include severe discomfort, redness, blurred vision, drainage, photosensitivity, and a white patch on the cornea.
- Slit-lamp examination, Gram stain and culture of the cornea are used to make the diagnosis.
Viral keratitis:
- Agents include herpes simplex viruses (HSV-1 and HSV-2), as well as varicella-zoster virus.
- Symptoms include pain, redness, impaired vision, tears, and dendritic ulcers (visible with fluorescein staining).
- Diagnosis: Slit-lamp examination with fluorescein staining, followed by PCR for viral DNA.
Fungal keratitis:
- Agents include Fusarium, Aspergillus, and Candida.
- Symptoms include pain, redness, impaired vision, drainage, and a feathery-edged corneal ulcer.
- Diagnosis: Fungal culture via corneal scraping, specific staining procedures (e.g., KOH prep), and potentially PCR.
Acanthamoeba keratitis:
- Agents: Acanthamoeba species are frequently linked to contact lens use and exposure to contaminated water.
- Symptoms include severe pain, redness, blurred vision, tears, and ring-shaped corneal infiltrates.
- Diagnosis methods include confocal microscopy, corneal scraping, and PCR.
3. Endophthalmitis
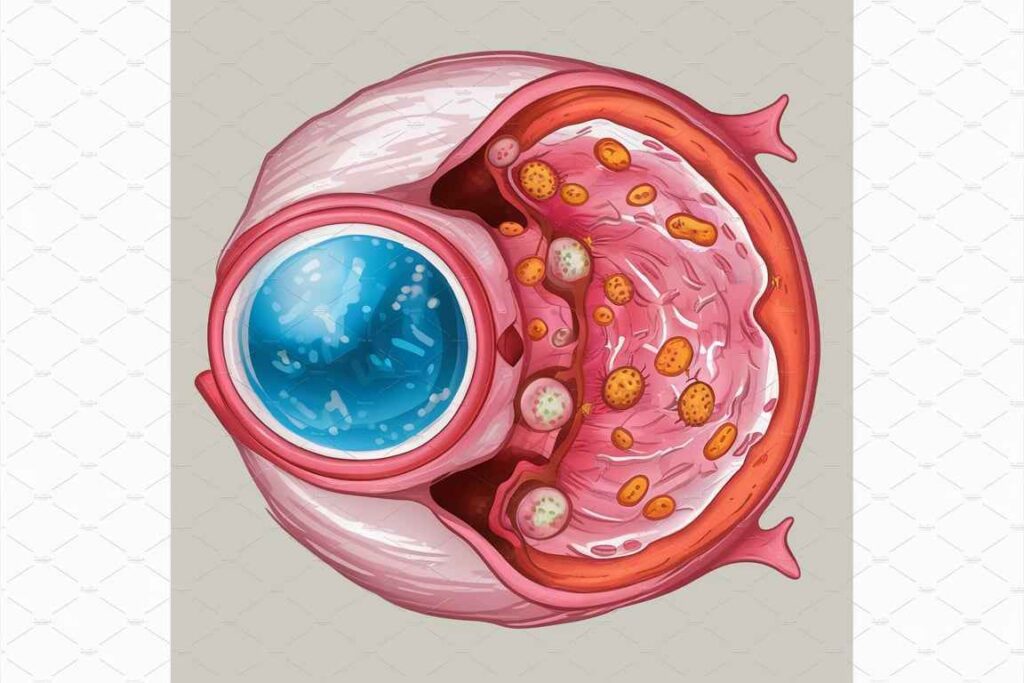
Types and Causes:
Exogenous endophthalmitis:
- Agents include Coagulase-negative staphylococci, Staphylococcus aureus, Streptococcus species, Gram-negative bacilli, and fungus (such as Candida).
- Symptoms include severe eye pain, visual loss, redness, swelling of the eyelids, and hypopyon (pus in the eye’s anterior chamber).
- Vitreous or aqueous fluid aspiration for Gram stain, culture, PCR, and blood cultures if systemic dissemination is indicated.
Endogenous endophthalmitis.
- Agents include Staphylococcus aureus, Streptococcus species, Gram-negative bacilli, and Candida species.
- Symptoms: Similar to exogenous endophthalmitis, but with systemic indications such as fever and malaise.
- Diagnosis: Similar to exogenous endophthalmitis, with blood cultures and imaging techniques (ultrasound, MRI) to assess the amount of infection.
4. Blepharitis
Types and Causing Agents:
Anterior blepharitis:
- Agents include Staphylococcus aureus, seborrheic dermatitis, and Demodex mites.
- Symptoms include redness, swelling, itching, burning, crusting around the base of the eyelashes, and flaky skin.
- Diagnosis: Clinical examination followed by a microscopic examination of the eyelash bases for mites.
Posterior blepharitis:
- Agents: Meibomian gland dysfunction (often linked with rosacea) and bacterial overgrowth.
- Symptoms included redness, swelling, itching, burning, meibomian gland obstruction, and oily or foamy tear film.
- Diagnosis: Clinical examination, including meibomian gland expression to assess secretions.
General Diagnostic Methods:
Clinical Exam:
- Visual examination reveals redness, swelling, discharge, crusting, and structural anomalies.
- Slit-lamp examination provides a detailed picture of the eye’s structures, which aids in the detection of ulcers, infiltrates, and other abnormalities.
Microbiological tests:
- Swabs and Cultures: Gather samples from the conjunctiva, cornea, or intraocular fluids.
- Gram stain is used to identify bacterial morphology and distinguish between Gram-positive and Gram-negative bacteria.
- Special Stains: To detect fungus and Acanthamoeba (e.g., KOH prep, Giemsa stain).
- PCR detects pathogen-specific DNA or RNA, which is very important for viruses and difficult-to-culture organisms.
Imaging techniques:
- Confocal microscopy is a high-resolution imaging technique that is particularly beneficial for identifying Acanthamoeba keratitis.
- Ultrasound: Examines inside eye structures; beneficial in serious illnesses such as endophthalmitis.
- CT/MRI provides precise imaging of the orbit and adjacent structures, which is useful in severe or difficult infections.
Blood test:
- Blood cultures are necessary in suspected endogenous endophthalmitis to detect systemic infection.
- General Blood Tests: A complete blood count (CBC) is performed to look for evidence of systemic infection or inflammation (such as an elevated white blood cell count).
Frequently Asked Question
What is an eye infection ?
An eye infection is an inflammatory disorder caused by bacteria, viruses, fungus, or parasites that can produce redness, swelling, pain, discharge, and reduced vision, depending on the kind and degree of the infection.
What are the types of eye infection?
The types of eye infection are
1. Conjunctivitis (Pink Eye)
2. Keratitis
3. Blepharitis
4. Endophthalmitis
Related Article
Specimen for Laboratory diagnosis of Central Nervous System Infections