Introduction
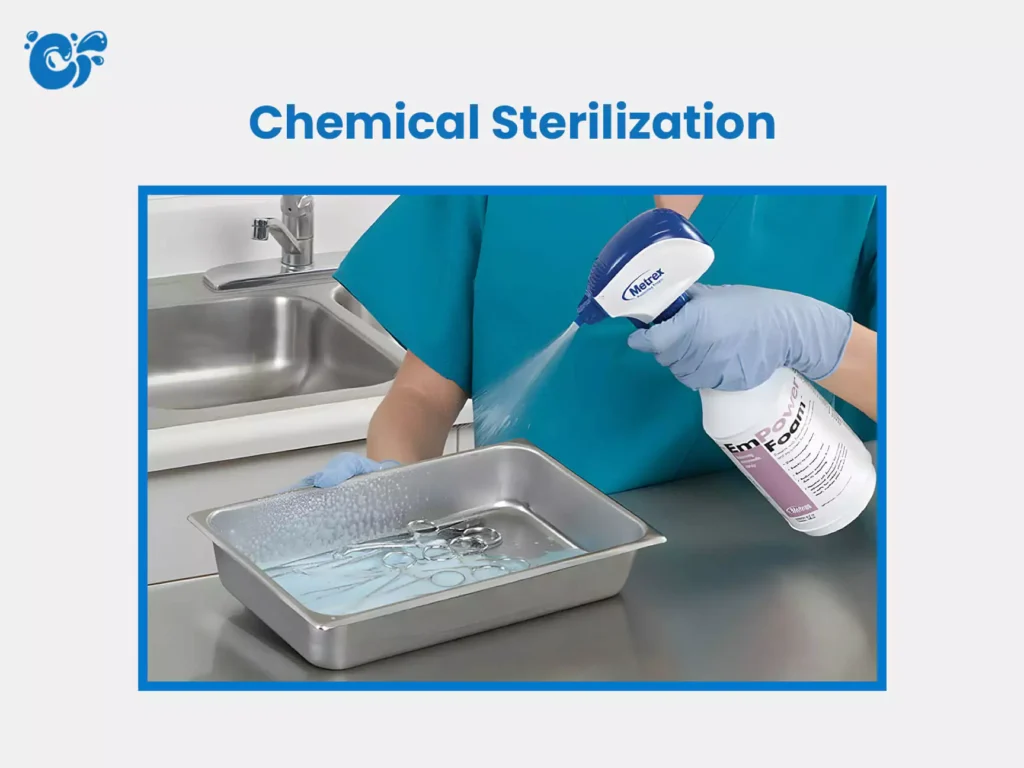
Chemical sterilization is the process of destroying all forms of microbial life, including bacteria, viruses, fungi, and spores, using chemical agents. It is used especially for heat-sensitive instruments and materials. Sterilization is the complete removal or destruction of all forms of microbial life, including bacteria, viruses, fungi, and spores. It is an essential process in healthcare, laboratories, food industries, and pharmaceutical production to ensure safety and prevent infections or contamination. While physical methods such as heat (autoclaving or dry heat) and radiation are widely used, chemical methods of sterilization play a crucial role, especially when heat-sensitive instruments or materials are involved.

Chemical sterilization methods use disinfectants or sterilants in either gaseous or liquid form. These chemicals penetrate and destroy microorganisms through different mechanisms, such as disrupting cell walls, denaturing proteins, or interfering with essential cellular processes.
This document provides a detailed and simplified explanation of the gaseous and liquid chemical sterilization methods, their types, mechanisms, applications, advantages, disadvantages, and safety concerns.
Table of Contents
1. Overview of Chemical Sterilization
Chemical sterilization involves using chemicals to eliminate all living organisms, especially microbial spores, which are the most resistant forms of life. It is typically used when physical methods cannot be applied, such as for:
- Heat-sensitive medical instruments (e.g., endoscopes)
- Plastic and rubber items
- Catheters
- Some pharmaceutical products
The two main forms are:
- Gaseous chemical sterilization
- Liquid chemical sterilization
Let’s explore both in detail.
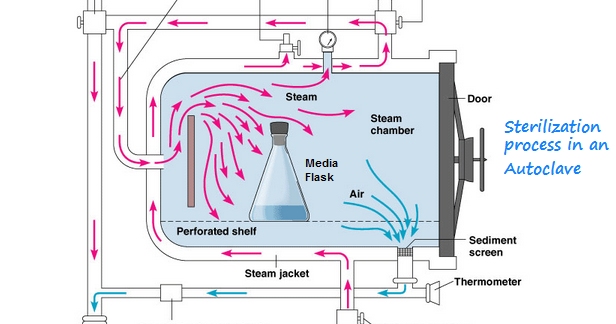
2. Gaseous Chemical Sterilization
Definition
Gaseous sterilization involves the use of volatile or vaporized chemical agents that are capable of penetrating materials and killing all forms of microbial life, including spores.
Common Gaseous Sterilants
a. Ethylene Oxide (EtO)
- Mechanism: Alkylates proteins, DNA, and RNA of microorganisms, rendering them inactive.
- Use: Commonly used in hospitals and medical industries for sterilizing surgical instruments, plastic devices, electronics, and heat/moisture-sensitive materials.
- Conditions: Sterilization typically occurs at 30–60°C with 30–90% relative humidity.
b. Formaldehyde Gas
- Mechanism: Cross-links proteins and nucleic acids, leading to microbial death.
- Use: Used for sterilizing rooms, cabinets, and biological safety equipment.
- Form: Can be used in vapor form or as paraformaldehyde (a solid that releases formaldehyde gas when heated).
c. Hydrogen Peroxide Vapor (HPV)
- Mechanism: Produces free radicals that damage cellular components.
- Use: Rapid sterilization of rooms, operating theaters, and sensitive medical devices.
d. Ozone (O₃)
- Mechanism: Oxidizes cellular enzymes and disrupts membranes.
- Use: Used for sterilizing medical equipment and water systems.
Advantages of Gaseous Sterilization
- Effective against all microorganisms, including spores
- Suitable for delicate and heat-sensitive instruments
- Can sterilize packaged items
- Reaches all surfaces, including complex instrument lumens
Disadvantages
- Toxicity: Many gaseous sterilants (e.g., EtO, formaldehyde) are harmful to health and require aeration after use
- Long cycle time (EtO can take several hours to complete)
- Flammability and explosion risk (EtO is highly flammable)
- High installation and operating cost
Safety Measures
- Proper ventilation and exhaust systems
- Personal protective equipment (PPE)
- Gas leak detectors and alarms
- Compliance with occupational safety guidelines (e.g., OSHA, EPA)
3. Liquid Chemical Sterilization
Definition
Liquid sterilization involves immersing objects in chemical solutions that destroy all microbial life, including spores, usually over a prolonged contact time.
Common Liquid Chemical Sterilants
a. Glutaraldehyde (2% solution)
- Mechanism: Cross-links proteins, affecting microbial enzymes and nucleic acids
- Use: Sterilization of surgical tools, endoscopes, respiratory equipment
- Time: Typically requires 10–12 hours for sterilization; shorter times achieve high-level disinfection
b. Peracetic Acid
- Mechanism: Oxidizes vital cellular components like proteins and enzymes
- Use: Used in automated systems for endoscopes, hemodialysis equipment
- Time: Rapid action (effective in 30–60 minutes)
c. Hydrogen Peroxide (H2O2) Liquid
- Mechanism: Releases reactive oxygen species that damage cellular contents
- Use: Surface sterilization, reusable medical devices
- Concentration: Typically 6–25%
d. Formalin (Formaldehyde in aqueous solution)
- Mechanism: Cross-links proteins
- Use: Tissue preservation and occasional surface sterilization
- Note: Has strong odor and is carcinogenic; use with caution
e. Chlorine Compounds (e.g., Sodium Hypochlorite)
- Mechanism: Strong oxidizer that disrupts cell membranes and enzymes
- Use: Surface and water sterilization
- Limitation: Corrosive and less effective in the presence of organic matter
Steps in Liquid Chemical Sterilization
- Cleaning: Thorough removal of organic/inorganic debris
- Immersion: Submerging instruments fully in the sterilant
- Contact Time: Ensuring adequate exposure (varies by chemical)
- Rinsing: Using sterile water to remove residual chemicals
- Drying and Storage: Avoiding recontamination
Advantages of Liquid Chemical Sterilization
- Ideal for instruments that cannot withstand high heat
- Can sterilize both interior and exterior surfaces
- Some agents (like peracetic acid) act quickly
- Convenient for small clinics and field settings
Disadvantages
- Chemical exposure risks to personnel
- Incomplete sterilization if not used properly
- Corrosive or damaging to certain materials
- Items cannot be stored sterile unless sealed immediately
- Requires careful rinsing to remove toxic residues
Precautions and Safety
- Use PPE (gloves, masks, eye protection)
- Adequate ventilation in sterilization areas
- Use validated protocols and exposure times
- Ensure proper rinsing to remove chemical residues
4. Comparison: Gaseous vs Liquid Chemical Sterilization
| Feature | Gaseous Sterilization | Liquid Sterilization |
|---|---|---|
| Physical State | Gas/Vapor | Liquid |
| Suitable For | Heat-sensitive instruments | Heat-sensitive, immersible items |
| Penetration | Excellent (reaches all areas) | Limited to surfaces in contact |
| Sterilization Time | Long (hours) | Variable (minutes to hours) |
| Residue Removal | Requires aeration | Requires rinsing |
| Safety Concern | Toxic gases | Chemical burns, toxic residues |
| Cost | Higher (equipment-intensive) | Moderate (depends on chemical) |
| Reusability | Equipment is reusable | Chemicals may degrade over time |
5. Applications of Chemical Sterilization
- Hospitals and Clinics:
- Endoscopes, surgical instruments, catheters
- Laboratories:
- Culture media, biosafety cabinets
- Pharmaceutical Industry:
- Sterilization of drug containers, vials
- Food Industry:
- Sterilization of packaging material and equipment
- Water Treatment Plants:
- Disinfection using chlorine or ozone
6. Challenges and Considerations
- Material Compatibility: Not all materials can withstand certain chemicals
- Environmental Impact: Some sterilants can be harmful if not properly disposed
- Worker Safety: Proper training and PPE are essential to avoid exposure
- Regulatory Compliance: Follow guidelines from health authorities like WHO, CDC, OSHA
- Validation and Monitoring: Use indicators (chemical and biological) to ensure effectiveness
7. Future Trends in Chemical Sterilization
- Green Sterilants: Development of environmentally friendly, non-toxic agents
- Automated Systems: Integration of robotics and smart sensors
- Shorter Cycles: New chemicals with faster action
- Improved Safety: Reduction in hazardous by-products
- Hybrid Techniques: Combining chemicals with physical methods like UV or heat
Conclusion
Chemical methods of sterilization, both gaseous and liquid, are indispensable tools in modern healthcare and industrial settings. They provide safe and effective sterilization for heat-sensitive and complex instruments that cannot be sterilized by physical means. Understanding their mechanisms, proper usage, advantages, and limitations helps ensure safety for patients, healthcare workers, and consumers.
While gaseous methods offer excellent penetration and are suitable for packaged items, liquid methods are versatile and accessible for many clinical settings. However, both require careful handling, adherence to protocols, and safety measures to avoid risks to human health and the environment.
As technology advances, the chemical sterilization field continues to evolve toward safer, more efficient, and eco-friendly solutions — making our environments cleaner and safer.
FREQUENTLY ASKED QUESTIONS
What is chemical sterilization?
Chemical sterilization is the process of destroying all forms of microbial life, including bacteria, viruses, fungi, and spores, using chemical agents. It is used especially for heat-sensitive instruments and materials.
What are the two main types of chemical sterilization?
The two main types are:\n- Gaseous sterilization (using chemical gases or vapors)\n- Liquid sterilization (using chemical solutions for immersion)
Are there any risks with using gaseous sterilants?
Yes. Many gaseous agents (like EtO and formaldehyde) are toxic, flammable, and require careful handling, proper ventilation, and post-sterilization aeration.
Related Articles