Cell proliferation is a fundamental biological process essential for growth, development, and maintenance of all multicellular organisms. It involves the controlled division and multiplication of cells to replace damaged tissues, maintain organ function, and ensure the survival of organisms throughout their lifespan.
Understanding the mechanisms of cell proliferation is crucial not only in basic cell biology but also in medical research and clinical practice. It plays a central role in fields like cancer biology, regenerative medicine, and immunology. Modern healthcare and scientific research continuously explore this process to develop effective treatments for diseases associated with abnormal cell growth.
Summary of Cell Proliferation
- Cell proliferation is the process by which cells divide and multiply, playing a crucial role in growth, tissue repair, and maintenance.
- This process is carefully regulated by the cell cycle, signaling pathways, and regulatory proteins to maintain healthy tissue function.
- Abnormal cell proliferation leads to diseases like cancer and fibrosis, while controlled proliferation is essential in therapies like regenerative medicine and immunotherapy.
Table of Contents
Importance of Understanding Cell Proliferation in Biology and Medicine
Studying cell proliferation provides valuable insights into how tissues regenerate, how immune responses are triggered, and how organisms develop from a single fertilized egg. It also helps uncover the molecular basis of diseases like cancer, where normal control of cell division is lost.
In medicine, controlling or stimulating cell proliferation is vital for procedures such as wound healing, organ regeneration, and immunotherapy. Therapeutic interventions often target the molecular machinery regulating this process, making it a cornerstone concept in modern medical science.
Brief Overview of Its Applications in Research and Healthcare
Applications of cell proliferation research extend far beyond cancer studies. In tissue engineering, for instance, researchers stimulate the proliferation of stem cells to develop artificial organs. In immunotherapy, controlled proliferation of immune cells enhances the body’s ability to fight infections and malignancies.
Additionally, pharmaceutical companies rely on proliferation assays to screen new drugs for cytotoxicity or regenerative potential. Cell proliferation studies have also contributed to breakthroughs in aging research, chronic inflammatory conditions, and genetic therapies.
What is Cell Proliferation?
Before understanding how it works and why it matters, it’s important to define the concept clearly and explore its biological significance.
Definition of Cell Proliferation
Cell proliferation refers to the process by which cells undergo division, resulting in the formation of two identical daughter cells. This process ensures tissue growth, repair, and replacement throughout the organism’s life. It involves a series of tightly regulated molecular events known as the cell cycle.
The outcome of cell proliferation is either the generation of more identical cells for tissue maintenance or the creation of specialized cells when followed by differentiation. Its regulation is vital for maintaining tissue homeostasis and preventing uncontrolled growth.
The Biological Purpose of Cell Proliferation
The primary biological purpose of cell proliferation is to support organismal growth, replace aged or damaged cells, and maintain tissue integrity. In developing embryos, proliferation contributes to rapid increases in cell number, forming tissues and organs.
In adults, proliferation balances cell loss due to injury, wear, and tear, ensuring organs continue to function properly. This is especially significant in high-turnover tissues such as the skin, gut epithelium, and blood.
Phases of the Cell Cycle Explained
The cell cycle is a series of phases through which a cell progresses to replicate its DNA and divide. Each phase has distinct molecular events and regulatory controls ensuring the fidelity of division.
The phases include:
- G1 Phase (Gap 1): The cell grows and prepares the necessary components for DNA replication.
- S Phase (Synthesis): The cell duplicates its genetic material.
- G2 Phase (Gap 2): The cell continues to grow and prepares for mitosis.
- M Phase (Mitosis): The cell divides its nucleus and cytoplasm, forming two daughter cells.
- G0 Phase: A resting state where cells temporarily or permanently exit the cycle.
Proper control of these phases is crucial to avoid mutations, uncontrolled proliferation, or cell death.
Mechanisms Regulating Cell Proliferation
Cell proliferation is tightly regulated by a network of proteins, signaling molecules, and checkpoints that ensure cells divide only when appropriate. Disruption in this regulation can lead to diseases like cancer.
Key Regulatory Proteins and Checkpoints
Cyclins and cyclin-dependent kinases (CDKs) are the main proteins driving the cell cycle. Cyclins bind CDKs to form active complexes that propel the cell from one phase to the next. Specific checkpoints (G1, G2, and metaphase) assess whether the cell is ready to proceed, checking for DNA damage, correct replication, and spindle alignment.
Tumor suppressor proteins like p53 halt the cycle if errors are detected, initiating repair or triggering cell death if damage is irreparable. The interplay of these molecules ensures cells proliferate accurately and safely.
Role of Growth Factors and Cytokines
External signals such as growth factors (e.g., EGF, PDGF) and cytokines regulate proliferation by binding to cell surface receptors. This activates intracellular signaling cascades that modulate gene expression, protein synthesis, and ultimately, cell cycle progression.
Growth factors play an especially important role in wound healing, immune responses, and embryonic development, while cytokines are critical in immune cell proliferation during infection and inflammation.
Signal Transduction Pathways in Proliferation
Intracellular signal transduction pathways such as the MAPK/ERK pathway, PI3K/Akt pathway, and JAK/STAT pathway transmit signals from growth factors and cytokines to the nucleus. These pathways activate transcription factors that control the expression of genes involved in proliferation, survival, and differentiation.
Aberrations in these pathways often result in excessive or insufficient cell proliferation, contributing to diseases like cancer, autoimmune disorders, or degenerative diseases.
Techniques to Measure Cell Proliferation
Quantifying cell proliferation is essential in both research and clinical diagnostics. Several assays have been developed to evaluate cell growth under different conditions.
Overview of Cell Proliferation Assays
Cell proliferation assays assess the number of actively dividing cells or their DNA synthesis rate. They help determine the cytotoxicity of drugs, evaluate growth factor activity, or monitor immune responses.
Assays are generally classified into metabolic activity-based, DNA synthesis-based, membrane labeling-based, and viability-based methods.
Common Methods
MTT and MTS Assays

These colorimetric assays measure cellular metabolic activity, which correlates with proliferation. Living cells convert MTT or MTS reagents into formazan crystals, measured spectrophotometrically.
BrdU (Bromodeoxyuridine) Incorporation Assay

BrdU is a thymidine analog incorporated into newly synthesized DNA during the S phase. Detection using anti-BrdU antibodies quantifies DNA synthesis and hence proliferation.
CFSE (Carboxyfluorescein Succinimidyl Ester) Staining
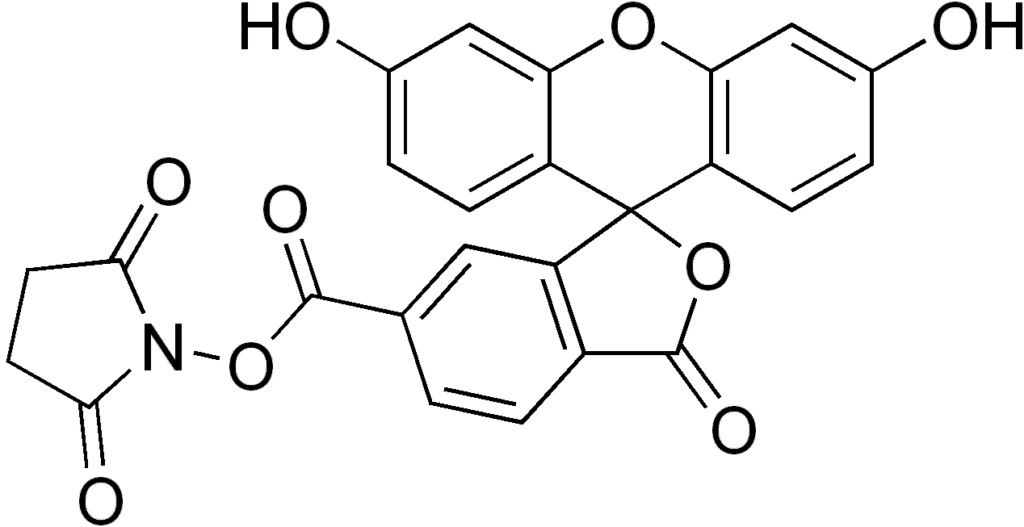
CFSE is a fluorescent dye that binds intracellular proteins. With each cell division, the fluorescence intensity halves, enabling researchers to track multiple cell divisions by flow cytometry.
Ki-67 Immunostaining
Ki-67 is a nuclear protein present during active phases of the cell cycle but absent in resting cells. Immunohistochemical detection of Ki-67 provides a reliable proliferation index in tissues and tumors.
Trypan Blue Exclusion Method
This viability assay distinguishes between live (unstained) and dead (stained) cells, indirectly reflecting proliferation by assessing cell viability over time.
Differentiation vs. Proliferation
While closely linked, cell proliferation and differentiation serve distinct biological functions. Understanding their relationship is vital in stem cell research, cancer biology, and tissue engineering.
Definition of Cell Differentiation
Cell differentiation is the process by which unspecialized cells acquire specialized functions and structures. Differentiated cells form the diverse tissues and organs in the body, each with unique roles.
Unlike proliferating cells, differentiated cells often exit the cell cycle, although some retain the ability to divide when necessary, like hepatocytes and lymphocytes.
How Proliferation Leads to Differentiation
During development, stem cells proliferate extensively before receiving signals to differentiate into specific cell types. The decision to differentiate involves halting the cell cycle at certain checkpoints and activating lineage-specific genes.
Balancing proliferation and differentiation ensures tissues grow properly while preventing excessive, disorganized growth, a hallmark of cancer.
Stem Cells: Balancing Proliferation and Differentiation
Stem cells uniquely maintain the capacity for both self-renewal (proliferation) and differentiation. This dual ability is critical for tissue repair and regeneration throughout life.
Understanding how to manipulate this balance forms the basis of regenerative medicine and holds promise for treating degenerative diseases and injuries.
Clinical Relevance of Cell Proliferation
Understanding how cells proliferate is crucial in clinical medicine, where both excessive and insufficient cell division can lead to disease. Many pathological conditions are rooted in the disruption of normal proliferation, whether through genetic mutations, environmental factors, or immune system dysfunction.
Proliferation also plays a positive role in tissue repair and regeneration, and is carefully harnessed in medical treatments like cell-based therapies, organ regeneration, and wound healing interventions.
Role in Tissue Repair and Regeneration
After tissue injury, cell proliferation is activated to replace lost or damaged cells and restore normal tissue architecture. Growth factors like EGF, PDGF, and FGF stimulate local stem cells or surviving differentiated cells to re-enter the cell cycle, proliferate, and contribute to tissue repair.
In regenerative medicine, stem cells are cultured and expanded in vitro to produce large quantities of cells for transplantation therapies, helping treat conditions such as burns, bone fractures, and degenerative organ diseases.
Cell Proliferation in Cancer Biology
Cancer arises when the regulatory mechanisms controlling proliferation are disrupted, resulting in uncontrolled and abnormal cell division. Mutations in oncogenes, tumor suppressor genes, and regulatory proteins like p53 and Rb disrupt the cell cycle, enabling cells to evade apoptosis and continue dividing unchecked.
The study of proliferation markers like Ki-67 and assays such as BrdU incorporation has become essential for tumor grading, prognosis prediction, and treatment planning in oncology.
Proliferation in Developmental Biology
In embryology, controlled and rapid proliferation drives the formation of tissues, organs, and systems from a single fertilized egg. Specific signaling pathways regulate proliferation at different stages of development to ensure proper morphogenesis and differentiation.
Disruptions in these processes can result in congenital malformations or developmental disorders. Understanding these mechanisms improves prenatal diagnostics and interventions.
Diseases Linked to Abnormal Cell Proliferation
When cell proliferation is not properly regulated, it can lead to various diseases. Both hyperproliferation (excessive cell division) and hypoproliferation (inadequate cell division) contribute to distinct pathological conditions.
Cancer: The Classic Proliferation Disorder
Cancer is the most well-known disease of uncontrolled cell proliferation. Genetic mutations that activate oncogenes or deactivate tumor suppressor genes allow cells to escape normal regulatory checkpoints, divide excessively, and form tumors.
Metastasis, where cancer cells proliferate and spread to other parts of the body, remains one of the deadliest aspects of cancer, emphasizing the importance of understanding and targeting proliferation pathways in cancer therapy.
Psoriasis and Skin Disorders
In conditions like psoriasis, skin cells proliferate at an abnormally high rate, leading to thick, scaly patches on the skin. This is often driven by immune system dysfunction, which stimulates excessive growth factor production and accelerates keratinocyte proliferation.
Studying cell proliferation in skin disorders has guided the development of topical and systemic treatments aimed at slowing down epidermal turnover.
Cardiovascular Diseases
After a heart attack, cardiac muscle cells have limited capacity for proliferation, leading to scar formation rather than tissue regeneration. Research into enhancing cardiac cell proliferation holds potential for improving recovery and function after myocardial infarction.
Additionally, abnormal proliferation of vascular smooth muscle cells contributes to conditions like atherosclerosis and restenosis, making it a focus of cardiovascular research.
Fibrosis and Chronic Inflammatory Conditions
Fibrosis involves excessive proliferation of fibroblasts and deposition of extracellular matrix components, leading to organ scarring and dysfunction. Chronic inflammatory diseases like liver cirrhosis and pulmonary fibrosis result from ongoing cycles of inflammation, injury, and dysregulated proliferation.
Understanding these processes informs the development of anti-fibrotic therapies aimed at reducing pathological cell proliferation.
Modern Applications of Proliferation Research
With the growing understanding of cell proliferation mechanisms, modern medicine and biotechnology have harnessed this knowledge for a wide range of applications, from cancer treatments to tissue engineering.
Anti-Cancer Drug Screening
Pharmaceutical companies use cell proliferation assays to test the efficacy of new anticancer drugs. By observing how these drugs affect the proliferation rate of cancer cells, researchers can identify promising candidates for further development.
Assays like MTT, BrdU incorporation, and Ki-67 immunostaining are routinely used to determine whether a drug slows or halts cell division.
Regenerative Medicine and Tissue Engineering
Regenerative medicine relies on stimulating cell proliferation to repair or replace damaged tissues. Techniques involve expanding stem cells in the laboratory, differentiating them into specialized cells, and implanting them into patients.
Advances in tissue engineering aim to produce bioengineered organs and tissues by combining scaffolds with proliferating cells, potentially addressing organ shortage problems in transplantation medicine.
Immunotherapy and Immune Cell Proliferation
In immunotherapy, controlled proliferation of immune cells like T-cells enhances their ability to combat infections and cancers. Techniques such as adoptive T-cell therapy involve expanding patient-derived immune cells in the lab before reintroducing them to fight disease.
Understanding the signals that regulate immune cell proliferation improves the efficacy and safety of immunotherapeutic approaches.
Recent Advances in Cell Proliferation Assays
Technological progress has revolutionized how cell proliferation is measured, allowing more precise, high-throughput, and dynamic analyses.
High-Throughput Screening Methods
Automated systems now allow researchers to test thousands of compounds for their effects on cell proliferation simultaneously. These platforms use robotic pipetting, microplate readers, and advanced data analysis software to identify potential therapeutic agents quickly and efficiently.
Live-Cell Imaging Technologies
Live-cell imaging permits real-time observation of cell division under the microscope, providing insights into cell cycle kinetics, proliferation rates, and responses to drugs. Fluorescent dyes and markers like CFSE and Ki-67 enable continuous monitoring of proliferating cells over time.
CRISPR/Cas9 Applications in Proliferation Studies
Gene-editing technologies such as CRISPR/Cas9 have transformed cell proliferation research by allowing precise manipulation of genes involved in cell cycle regulation. Researchers can knock out oncogenes, activate tumor suppressors, or modify signaling pathways to study their effects on cell growth.
This has opened new avenues for identifying drug targets and developing gene-based therapies for proliferation-related diseases.
Ethical Considerations in Proliferation Research
While advances in cell proliferation research offer immense potential, they also raise important ethical questions, particularly when involving human stem cells or gene editing.
Use of Human Stem Cells
The use of human embryonic stem cells in research poses ethical challenges due to concerns about the destruction of potential human life. Alternative sources, like induced pluripotent stem cells (iPSCs), which are reprogrammed from adult cells, offer a less controversial option for studying proliferation.
Genetic Editing and Regulation
Gene-editing tools like CRISPR must be used responsibly to avoid unintended consequences. Manipulating proliferation pathways in human cells carries the risk of creating abnormal or tumorigenic cells, necessitating strict ethical oversight and regulatory control.
Conclusion
In summary, cell proliferation is a central process in biology and medicine, essential for growth, development, tissue maintenance, and repair. Its regulation involves a complex network of signals, proteins, and pathways that ensure precise control over cell division.
Abnormal proliferation leads to serious diseases such as cancer, fibrosis, and chronic inflammation, while controlled proliferation offers therapeutic opportunities in regenerative medicine and immunotherapy. Modern research techniques continue to refine our understanding of proliferation and offer hope for innovative treatments. As we advance into an era of personalized medicine and gene therapy, ethical considerations will remain integral to ensuring that cell proliferation research benefits humanity while minimizing potential risks.
Frequently Asked Questions (FAQ)
What factors influence cell proliferation rates?
Cell proliferation rates are influenced by growth factors, hormones, nutrients, oxygen supply, and genetic signals. Stress, infections, and damage can also speed up or slow down how quickly cells divide.
How is cell proliferation measured in a clinical setting?
In clinics, cell proliferation is often measured using markers like Ki-67 through tissue biopsies, or by tracking DNA synthesis with tests like BrdU labeling.
Can cell proliferation be artificially controlled?
Yes doctors and scientists can control cell proliferation using medications, radiation, or gene-editing tools. This is done to slow down unwanted cell growth in diseases like cancer or to boost it during wound healing and regenerative therapies.