In recent years, the global healthcare landscape has faced a rapidly growing challenge due to the emergence and spread of antimicrobial-resistant bacteria. Among these pathogens, Pseudomonas aeruginosa has gained particular attention because of its ability to acquire resistance mechanisms quickly and survive in diverse, often hostile, environments. One of the most concerning forms of resistance this bacterium displays is against carbapenems, which are often considered antibiotics of last resort for severe infections.
Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) infections are increasingly being reported in hospitals worldwide, especially in intensive care units and immunocompromised patient populations. These infections are associated with high morbidity, extended hospital stays, and significant healthcare costs, posing a critical public health concern.
Summary of Carbapenem-Resistant Pseudomonas aeruginosa (CRPA)
- Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) is a hospital-acquired, carbapenem-resistant Pseudomonas aeruginosa.
- It resists treatment via enzymes, efflux pumps, and biofilm formation.
- Managed with last-resort drugs and strict infection control.
Table of Contents
Definition of Carbapenem-Resistant Pseudomonas aeruginosa (CRPA)
Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) refers to strains of P. aeruginosa that demonstrate resistance to at least one of the carbapenem antibiotics, such as imipenem, meropenem, or doripenem. These antibiotics are part of the β-lactam class and are widely employed to treat multidrug-resistant Gram-negative bacterial infections, particularly when other treatment options have failed.
CRPA strains can develop resistance through both intrinsic factors inherent to the species and acquired mechanisms gained from other bacteria. This combination of adaptive traits makes CRPA a particularly dangerous pathogen, as it can resist multiple classes of antibiotics while persisting in harsh environments like hospital surfaces, medical devices, and moist clinical settings.
Characteristics of Pseudomonas aeruginosa
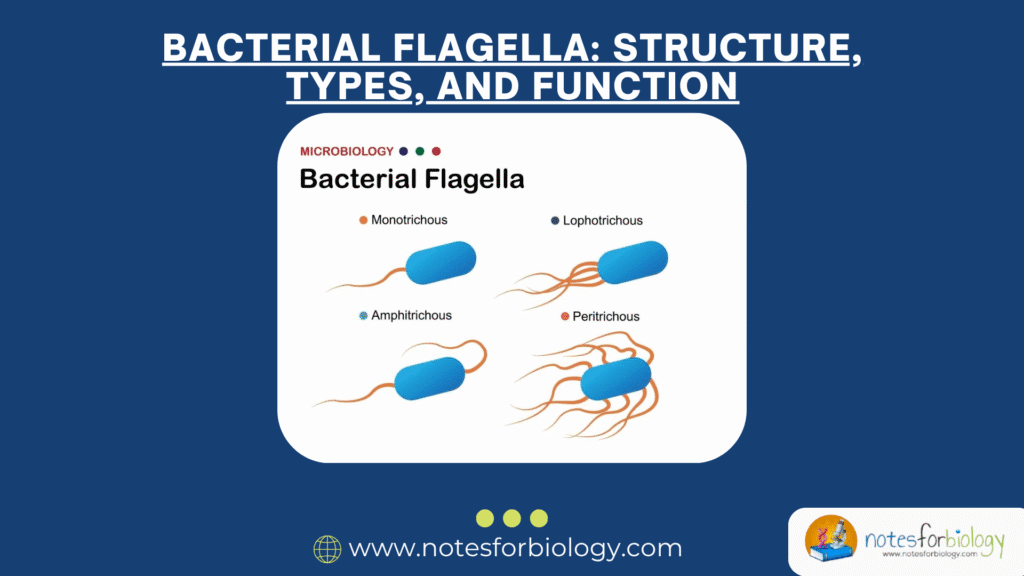
Pseudomonas aeruginosa is a Gram-negative, rod-shaped, non-fermenting, obligate aerobe, although it can survive anaerobic conditions when necessary. The bacterium is highly motile due to its polar flagella and is capable of forming biofilms, which contribute to its persistence in clinical environments and on indwelling medical devices.
Pseudomonas aeruginosa possesses several distinctive features that contribute to its pathogenicity and resilience:
Gram-Negative, Rod-Shaped Morphology
This bacterium is a Gram-negative, aerobic, rod-shaped bacillus equipped with a single polar flagellum, facilitating motility in aqueous environments.
Metabolic Versatility
It demonstrates remarkable metabolic adaptability, capable of surviving in diverse conditions including soil, water, medical devices, and even antiseptic solutions.
Opportunistic Pathogen
While typically harmless to healthy individuals, P. aeruginosa can cause severe infections in immunocompromised patients, burn victims, those with cystic fibrosis, and hospitalized individuals with invasive devices like catheters and ventilators.
Intrinsic and Acquired Resistance
The organism naturally exhibits resistance to many antibiotics through mechanisms like low outer membrane permeability and efflux pumps. It can also rapidly acquire resistance genes, further complicating treatment.
Mechanisms of Carbapenem Resistance in Pseudomonas aeruginosa
The resistance of Pseudomonas aeruginosa to carbapenem antibiotics is not attributable to a single pathway but involves several complex and overlapping mechanisms. These adaptive strategies make Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) particularly resilient against antibiotic therapy and challenging to manage in clinical settings.
Production of Carbapenemases
One of the foremost mechanisms responsible for carbapenem resistance is the production of carbapenem-hydrolyzing enzymes known as carbapenemases. These enzymes degrade carbapenems before they can interfere with bacterial cell wall synthesis, rendering the antibiotics ineffective.
Metallo-β-lactamases (MBLs), including Verona Integron-encoded MBL (VIM), Imipenemase (IMP), and New Delhi Metallo-β-lactamase (NDM), are among the most clinically significant. These enzymes are often encoded on mobile genetic elements such as plasmids, facilitating horizontal transmission of resistance genes within and between bacterial species.
Efflux Pump Overexpression
Another vital contributor to carbapenem resistance in P. aeruginosa is the overproduction of efflux pumps. These protein complexes expel antibiotics and other toxic substances from the bacterial cell, reducing the intracellular concentration of the drug to sub-lethal levels.
In CRPA, systems such as MexAB-OprM, MexXY-OprM, and MexCD-OprJ are commonly upregulated, leading to high levels of carbapenem resistance. Efflux pumps are significant because they can confer cross-resistance to multiple classes of antibiotics, complicating treatment strategies further.
Loss or Alteration of Porin Channels
Carbapenems typically enter the bacterial cell through outer membrane porins, particularly OprD. In CRPA, mutations or downregulation of the oprD gene lead to decreased expression or functional loss of the OprD porin.
This reduction in permeability hinders the antibiotic’s ability to reach its target site within the bacterial cell, allowing the bacterium to survive even in the presence of carbapenem concentrations that would typically be inhibitory.
Acquisition of Resistance Genes via Horizontal Gene Transfer
The transfer of genetic material between bacteria, known as horizontal gene transfer, plays a pivotal role in the rapid spread of carbapenem resistance. Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) can acquire resistance genes through plasmids, transposons, and integrons from other resistant organisms within the clinical environment.
This genetic exchange allows Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) strains to adapt swiftly to antimicrobial pressure and disseminate resistance traits both locally and globally.
Biofilm Formation and Its Role in Resistance
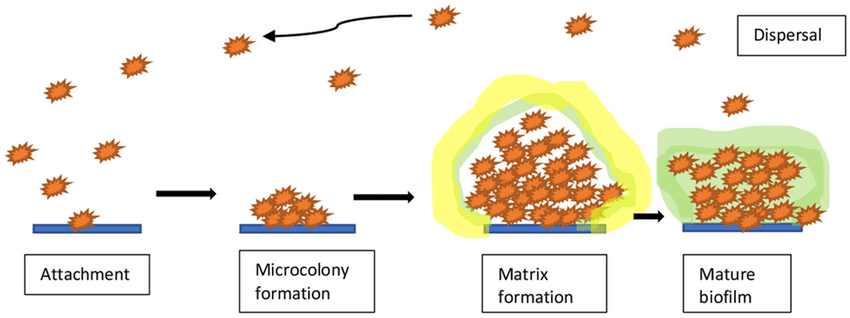
An often underappreciated aspect of CRPA’s resilience lies in its ability to form biofilms. Biofilms are structured communities of bacteria encased within a self-produced matrix of extracellular polymeric substances (EPS), which adhere to surfaces such as catheters, endotracheal tubes, and wound beds.
Within biofilms, bacteria exhibit altered phenotypes, including enhanced resistance to antibiotics and immune responses. This biofilm-associated resistance, combined with carbapenem resistance mechanisms, makes CRPA infections particularly difficult to eradicate using standard therapeutic regimens.
Structure and Composition
A biofilm is a structured, multicellular community of bacteria encased in a self-produced extracellular polymeric substance (EPS) composed of polysaccharides, proteins, lipids, and extracellular DNA.
Stages of Biofilm Development
The process involves several stages:
- Initial attachment to surfaces.
- Microcolony formation through bacterial aggregation.
- Biofilm maturation, with structured layers and channels.
- Dispersal, where bacteria detach and colonize new sites.
Biofilm-Associated Resistance Mechanisms
Biofilms contribute to antibiotic resistance through:
- Physical barrier effects, limiting antibiotic diffusion.
- Altered microenvironment (low oxygen, pH gradients) affecting drug activity.
- Slow-growing persister cells resistant to antibiotics.
- Enhanced horizontal gene transfer within the biofilm, spreading resistance genes.
Clinical Significance of Carbapenem-Resistant Pseudomonas aeruginosa (CRPA)
The impact of CRPA infections extends beyond the individual patient, affecting healthcare systems and public health infrastructures. Infections caused by CRPA are associated with high rates of morbidity, increased mortality, prolonged hospitalizations, and elevated healthcare expenses.
Respiratory Tract Infections
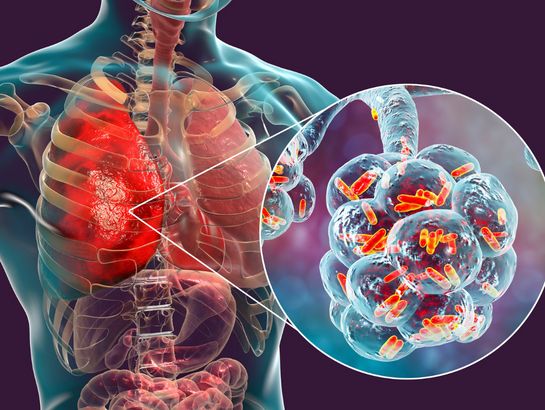
CRPA is a leading cause of hospital-acquired respiratory infections, especially ventilator-associated pneumonia (VAP) in intensive care settings. These infections are difficult to treat due to the limited number of effective antibiotics and the bacterium’s ability to persist in respiratory equipment and biofilms.
Bloodstream Infections
CRPA bacteremia is particularly dangerous, as it can rapidly progress to sepsis and septic shock. The prognosis is often poor, especially in neutropenic or immunocompromised patients, with mortality rates significantly higher than those associated with carbapenem-susceptible strains.
Urinary Tract and Wound Infections
CRPA can colonize and infect urinary catheters, surgical sites, and burn wounds. These infections are prone to recurrence, slow healing, and can lead to invasive complications such as osteomyelitis or bloodstream invasion.
Laboratory Diagnosis of Carbapenem-Resistant Pseudomonas aeruginosa (CRPA)
Timely and accurate identification of CRPA is essential for appropriate clinical management, infection control, and epidemiological surveillance. Several laboratory methods are used in tandem to confirm the presence of carbapenem resistance in P. aeruginosa isolates.
Antibiotic Susceptibility Testing
Standardized methods such as disk diffusion, broth microdilution, and automated systems (e.g., VITEK, BD Phoenix) are employed to assess the susceptibility profile of bacterial isolates. Determining minimum inhibitory concentrations (MICs) of carbapenems helps guide appropriate therapy.
Carbapenemase Detection Assays
Phenotypic tests like the Modified Hodge Test, Carba NP test, and EDTA-disk synergy test are used to detect the presence of carbapenemase enzymes. These tests are valuable in differentiating carbapenemase-producing isolates from those with other resistance mechanisms.
Molecular Diagnostics
PCR assays targeting carbapenemase-encoding genes (bla_VIM, bla_IMP, bla_NDM) offer rapid and highly specific results. Whole-genome sequencing (WGS) is increasingly applied for detailed characterization of resistance mechanisms and outbreak investigations.
Treatment Options for Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) Infections
Treating CRPA infections remains a significant challenge due to the scarcity of effective antibiotics and the bacterium’s multidrug resistance. Therapy often involves a combination of antimicrobial agents to maximize bacterial killing and prevent further resistance development.
Polymyxins
Polymyxin B and colistin are frequently considered last-line agents for CRPA infections. While effective, their nephrotoxicity and neurotoxicity limit their routine use, necessitating careful dosing and monitoring.
Ceftolozane-Tazobactam and Newer β-lactamase Inhibitor Combinations
Ceftolozane-tazobactam and ceftazidime-avibactam have shown promising activity against certain CRPA strains, particularly those lacking carbapenemases. These drugs offer improved outcomes and may be preferable in severe infections.
Adjunctive Agents
Depending on susceptibility results, aminoglycosides, fosfomycin, and fluoroquinolones may be considered in combination regimens. Selection should be guided by MIC values and clinical context.
Infection Control and Prevention Measures
Preventing the spread of Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) within healthcare facilities requires stringent infection control protocols and antimicrobial stewardship programs. Early identification and isolation of colonized or infected patients are crucial to containing outbreaks.
Hand Hygiene and Contact Precautions
Rigorous hand hygiene practices and use of personal protective equipment (PPE) like gloves and gowns are essential in preventing cross-transmission. Dedicated medical equipment for CRPA patients further minimizes infection risks.
Environmental Cleaning and Disinfection
Regular disinfection of patient rooms, intensive care units, and hospital equipment is critical to reducing environmental reservoirs of CRPA. Disinfectants effective against Gram-negative pathogens should be prioritized.
Surveillance and Reporting
Routine screening of high-risk patients and prompt reporting of Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) cases to infection control committees facilitate early outbreak detection and control measures.
Conclusion
Carbapenem-Resistant Pseudomonas aeruginosa (CRPA) represents a formidable challenge in modern clinical microbiology and infectious disease management. Its capacity to resist some of the most potent antibiotics, coupled with its adaptability and virulence, demands vigilant surveillance, robust infection control, and effective antimicrobial stewardship.
While current treatment options remain limited, advances in new antibiotic development, rapid diagnostic methods, and global collaboration offer hope in combating this serious public health threat.
Frequently Asked Questions (FAQ)
What is CRPA disease?
It’s an infection caused by Pseudomonas aeruginosa bacteria that are resistant to carbapenem antibiotics, often seen in hospitals.
What is carbapenem-resistant Pseudomonas?
It’s a strain of Pseudomonas aeruginosa that can survive carbapenem antibiotics, making infections hard to treat.
What are the top 3 antibiotics for Pseudomonas aeruginosa?
Commonly used options are piperacillin-tazobactam, ceftazidime, and meropenem (if the strain is still sensitive).