Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps it throughout the body. It is a vital indicator used to determine cardiovascular health. It is usually measured in millimeters of mercury (mmHg) and expressed as two numbers: systolic pressure and diastolic pressure. The systolic pressure (the higher number) indicates the pressure in the arteries while the heart beats, whereas the diastolic pressure (the lower number) indicates the pressure in the arteries when the heart is at rest between beats.
Table of Contents
Systolic Blood Pressure
It is the maximum pressure in the arteries as the heart beats and pumps blood through them. It represents the stress exerted on the artery walls during ventricular contraction (systole). Systolic pressure is the highest number in a Bp reading (e.g., 120 in 120/80 mmHg).
Diastolic Blood Pressure
It is the pressure in the arteries when the heart is at rest between beats, also known as diastole. During this period, the heart fills with blood, and the pressure exerted on the artery walls is known as diastolic pressure. It is the lower number in a Bp reading (for example, 80 in 120/80 mmHg).
Measurement
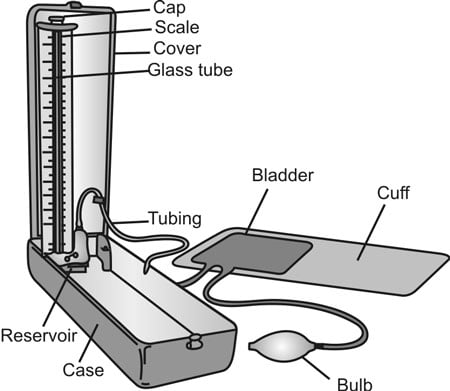
A sphygmomanometer is often used to monitor Bp. It consists of an inflatable cuff, a measuring unit (either mercury or aneroid), and a stethoscope.
The method includes the following steps:
Preparation: The patient should sit comfortably, with their arm supported at heart level. The cuff fits tightly around the upper arm.
Inflation: The cuff is inflated to a pressure greater than the expected systolic pressure, preventing blood flow in the artery.
Deflation and Measurement: The cuff steadily deflates. As the pressure drops, the examiner listens with a stethoscope or watches the display for Korotkoff sounds:
1. The first sound detected is systolic pressure.
2. The disappearance of sound signifies diastolic pressure.
Automated digital Bp monitors make this process easier by employing oscillometric detection techniques and delivering a digital readout of Bp measurements.
Mechanism
Several variables contribute to Bp regulation:
Cardiac output: It is the amount of blood that the heart pumps every minute. High cardiac output raises Bp.
Peripheral Resistance: The blood vessel’s resistance to blood flow. Blood pressure rises as vessels become narrower or more stiff (for example, as a result of arteriosclerosis).
Blood volume: It is the total amount of blood circulating within the vessels. High blood volume can raise blood pressure.
Viscosity of Blood: Thicker blood (greater viscosity) can lead to elevated blood pressure.
Elasticity of Arterial walls: Healthy, elastic arteries can readily expand and contract, which helps to keep blood pressure stable. Elasticity loss (for example, caused by age) might result in elevated blood pressure.
The nervous system, endocrine system, and kidneys interact in various ways to regulate blood pressure:
Nervous System: The autonomic nervous system (ANS) governs short-term changes in blood pressure via the sympathetic and parasympathetic branches. The baroreceptor reflex regulates blood pressure(Bp) by altering heart rate and artery diameter in response to arterial pressure variations.
Endocrine System: Hormones such as adrenaline, angiotensin II, and antidiuretic hormone (ADH) regulate bp by influencing heart rate, blood vessel tone, and blood volume.
Kidneys: The kidneys regulate long-term Bp using the renin-angiotensin-aldosterone system (RAAS), which controls blood volume and systemic vascular resistance.
Abnormal Blood Pressure
They are those that depart from the normal range deemed healthy for most persons. Bp is abnormal when it is either too high (hypertension) or too low (hypotension).
Hypotension
Hypotension occurs when Bp readings fall below the normal range, which is commonly characterized as:
Systolic: <90 mmHg
Diastolic: <60 mmHg
Causes:
1. Dehydration
2. Heart problems (such as bradycardia and heart failure)
3. Endocrine disorders (e.g., adrenal insufficiency)
4. Severe infection (Sepsis)
5. Blood loss
6. Certain medications (e.g., antihypertensive and diuretics)
Measures:
1. Increase fluid and salt intake.
2. Wearing compression stockings.
3. Medications (if needed) to raise blood pressure
4. Treating underlying conditions.
Hypertension
Hypertension is a condition in which blood pressure levels continuously exceed normal limits. It is classified into several stages:
Normal Bp: systolic <120 mmHg, diastolic <80 mmHg.
Elevated Bp: systolic 120-129 mmHg, diastolic <80 mmHg.
Stage 1 Hypertension: systolic 130-139 mmHg or diastolic 80-89 mmHg.
Stage 2 Hypertension: systolic ≥140 mmHg or diastolic ≥90 mmHg.
Hypertensive crisis: systolic >180 mmHg or diastolic >120 mmHg, requiring rapid medical treatment.
Causes:
1. Family history, aging
2. High salt, poor diet, inactivity, obesity
3. Chronic stress, tobacco use
4. Kidney disease, endocrine disorders
5. Certain drugs, preeclampsia
Measures:
1. Eat a low-salt, heart-healthy diet.
2. Engage in regular physical activity.
3. Take prescribed blood pressure medications.
4. Practice relaxation techniques and get adequate sleep.
5. Limit alcohol intake and quit smoking.
To conclude, Blood pressure is a critical indicator of cardiovascular health that is calculated by measuring the force of blood against artery walls during heartbeats and at rest. It is determined by cardiac output, vascular resistance, blood volume, and arterial flexibility. Accurate measurement and understanding of the regulatory mechanisms are critical for identifying and treating blood pressure-related disorders.
Frequently Asked Questions (FAQ)
What are the risk factors for hypertension?
Risk factors include genetics, age, poor diet, lack of exercise, obesity, stress, and smoking.
How often should an individual check their blood pressure?
It is recommended that you check your blood pressure at least once a year, or more frequently if directed by your healthcare practitioner.
What lifestyle adjustments can help you control hypotension?
Lifestyle adjustments include: stay hydrated, minimize extended periods of standing, eat smaller, more frequent meals, and avoid alcohol and caffeine.
Related Articles