Urinary tract infections (UTIs) are one of the most frequent bacterial infections seen in both community and hospital settings. They are particularly common in women, the elderly, and individuals with underlying health conditions such as diabetes.
Understanding the bacterial causes of UTIs is vital for effective diagnosis, appropriate treatment choices, and reducing the risk of serious complications. This article provides a detailed review of the key bacterial agents responsible for UTIs, their pathogenic mechanisms, diagnostic methods, and management strategies.
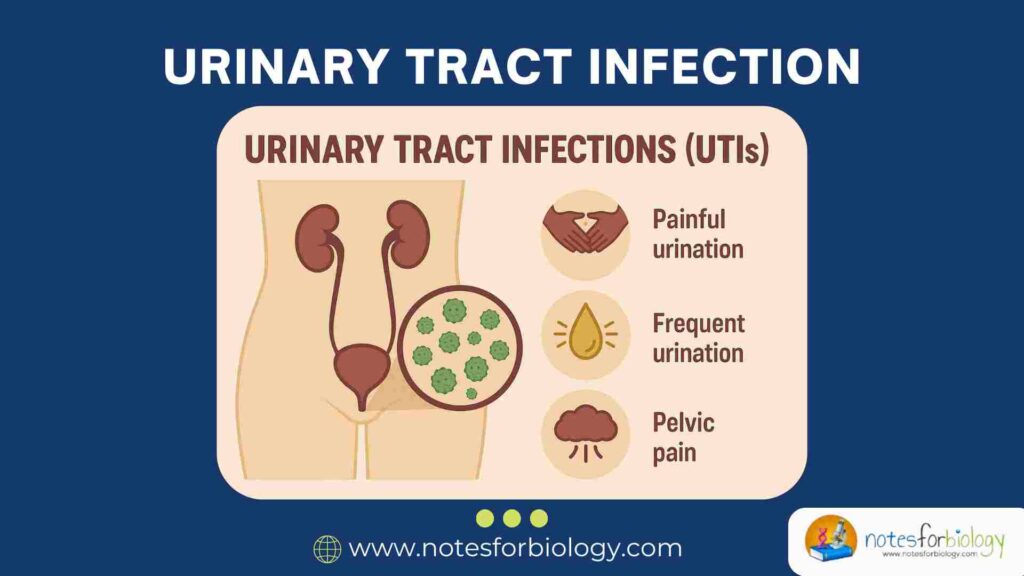
Summary of Urinary Tract Infections (UTIs)
- UTIs are common bacterial infections affecting the urinary system, with Escherichia coli (E. coli) being the leading cause, especially in women and hospitalized patients.
- Symptoms include painful, frequent urination and pelvic discomfort, and if untreated, UTIs can lead to serious complications like kidney infections and sepsis.
- Prompt diagnosis, appropriate antibiotics, and preventive measures such as good hygiene and adequate hydration are essential to manage and reduce UTI risks.
Table of Contents
Overview of Urinary Tract Infections (UTIs)
The urinary tract is a sterile system responsible for producing and expelling urine, but under certain conditions, it becomes vulnerable to bacterial invasion. UTIs occur when bacteria colonize the urethra and ascend to infect other parts of the urinary tract, causing inflammation and tissue damage.
These infections range from mild cases affecting the lower urinary tract to severe infections involving the kidneys and bloodstream. Early detection and appropriate therapy are essential to prevent further complications.
Why Understanding Bacterial Causes is Important
Identifying the exact bacterial pathogen behind a UTI enables clinicians to tailor antibiotic treatment to the infection. This reduces the risk of drug resistance and recurrent infections, especially in hospital settings where resistant bacteria are prevalent.
Recognizing bacterial causes also helps inform public health strategies aimed at improving infection control, hygiene practices, and preventive care protocols.
What is a Urinary Tract Infection (UTI)?
A urinary tract infection refers to an infection in any part of the urinary system caused by the growth and multiplication of microorganisms, predominantly bacteria. These infections can affect both men and women, though they are much more common in females due to anatomical differences.
UTIs not only cause discomfort and inconvenience but also pose significant health risks if left untreated, as the infection can spread to the kidneys and even enter the bloodstream.
Definition and Affected Organs
A UTI is defined as an infection affecting the urinary organs, which include the urethra, bladder, ureters, and kidneys. Although most UTIs involve the lower urinary tract, upper tract infections tend to be more dangerous.
The primary role of the urinary tract is to produce, store, and remove urine, and any infection in this system can disrupt these processes and cause inflammatory symptoms.
Types of UTIs: Cystitis, Urethritis, Pyelonephritis
- Cystitis is an infection of the bladder, often presenting with pelvic pain, frequent urination, and discomfort during urination.
- Urethritis involves the inflammation of the urethra, typically causing burning or pain during urination.
- Pyelonephritis affects the kidneys, presenting with flank pain, fever, and nausea, and may require urgent hospitalization for treatment.
Symptoms of Urinary Tract Infections
The symptoms of UTIs can vary based on the site of infection and severity but generally include a persistent urge to urinate and pain during urination.
Other signs may include cloudy or foul-smelling urine, pelvic discomfort, and, in more severe cases, fever and flank pain. Recognizing these symptoms promptly can aid in early diagnosis and prevent complications.
How Bacteria Cause Urinary Tract Infections
Bacteria responsible for UTIs enter the body through the urethra and migrate into the bladder, where they multiply and trigger an inflammatory response. Certain bacteria possess specialized surface structures that help them adhere to the urinary tract’s epithelial lining.
Once established, these bacteria can form biofilms and evade immune defenses, increasing their ability to persist within the urinary system.
Pathogenesis of Bacterial Infections in the Urinary Tract
The pathogenesis of UTIs involves bacterial colonization of the periurethral area, followed by ascent into the bladder and potentially the kidneys. Adhesion to urothelial cells is a critical first step, often mediated by fimbrial adhesins.
After attachment, bacteria multiply, triggering a host immune response characterized by white blood cell infiltration and cytokine release, leading to inflammation and tissue damage.
Common Entry Routes and Risk Factors
The most frequent route of infection is ascending infection, where bacteria move from the external environment to the bladder. Risk factors include poor hygiene, frequent sexual activity, urinary catheter use, and anatomical anomalies.
Other contributors are weakened immune defenses, postmenopausal changes, and underlying diseases like diabetes, which can impair the body’s ability to clear bacterial invaders.
Most Common Bacteria Causing Urinary Tract Infections
Several bacterial species are associated with UTIs, though a few predominate in both community and hospital settings. Their ability to form biofilms, resist antibiotics, and produce virulence factors makes them challenging pathogens to manage.
Identifying the species responsible for infection is crucial for selecting appropriate treatment and preventing recurrent or complicated cases.
Escherichia coli (E. coli)

E. coli is the leading cause of UTIs globally, accounting for the majority of both uncomplicated and complicated cases.
Prevalence and Role
E. coli naturally resides in the gastrointestinal tract but can easily reach the urethra and bladder, especially in females due to anatomical proximity. Its prevalence and adaptability make it the primary uropathogen encountered in clinical practice.
Virulence Factors and Adhesion Mechanisms
E. coli expresses various virulence factors such as P fimbriae, type 1 pili, and toxins like hemolysin, which enhance its ability to colonize and damage the urinary tract epithelium. These structures enable it to evade the immune system and persist in urinary tissues.
Klebsiella pneumoniae

This bacterium is a major cause of healthcare-associated UTIs, particularly in catheterized or immunocompromised individuals.
Common in Hospital-Acquired Urinary Tract Infections
Klebsiella is frequently isolated from catheter-related infections and intensive care units, where it can persist in moist environments and on medical equipment.
Antibiotic Resistance Issues
Klebsiella species often exhibit multidrug resistance, especially strains producing extended-spectrum beta-lactamases (ESBLs), limiting treatment options and increasing morbidity rates.
Proteus mirabilis
A motile, urease-producing bacterium, Proteus mirabilis is a frequent cause of complicated urinary tract infections, particularly those involving long-term catheterization.
Its unique biochemical properties allow it to alter the urinary environment, facilitating persistent infection and stone formation.
Associated with Kidney Stones
Proteus infections are commonly associated with the formation of struvite stones in the kidneys or bladder. These stones form when Proteus hydrolyzes urea into ammonia, alkalinizing the urine and promoting mineral precipitation.
Urease Production and Alkaline Urine
By producing the enzyme urease, Proteus mirabilis increases urine pH, creating an alkaline environment favorable to bacterial survival and stone formation. This biochemical activity complicates infection management and often necessitates combined antimicrobial and surgical interventions.
Enterococcus faecalis
A Gram-positive bacterium, Enterococcus faecalis frequently causes recurrent UTIs, particularly in elderly patients or those with underlying urological conditions.
Common in Recurrent Infections
Enterococcus is notable for its ability to persist in the urinary tract and healthcare settings, causing chronic and relapsing infections. It frequently colonizes indwelling urinary devices and post-surgical sites.
Challenges in Treatment
Treatment of Enterococcus infections is difficult because of intrinsic resistance to many antibiotics such as cephalosporins and some beta-lactams. Multidrug-resistant strains further complicate therapy, requiring the use of specific agents like vancomycin or linezolid.
Pseudomonas aeruginosa
An opportunistic, Gram-negative pathogen, Pseudomonas aeruginosa causes UTIs in hospitalized and immunocompromised patients, often associated with indwelling catheters or structural urinary abnormalities.
Opportunistic Pathogen
Though relatively rare in healthy individuals, Pseudomonas thrives in hospital environments and on medical equipment, making it a frequent cause of nosocomial infections, especially in intensive care units.
Complicated and Chronic Urinary Tract Infections
Pseudomonas forms biofilms on catheters and urinary tract surfaces, making infections difficult to eradicate. Its high resistance to multiple antibiotics limits treatment options, often necessitating combination therapies.
Staphylococcus saprophyticus
A Gram-positive coccus, Staphylococcus saprophyticus is a common cause of community-acquired UTIs, particularly in sexually active young women.
Common in Young Women
It accounts for a notable percentage of UTI cases in healthy females, second only to E. coli in prevalence. Its ability to adhere to urothelial cells enables it to initiate infection following sexual activity or hormonal changes.
Community-Acquired Urinary Tract Infections
Unlike other staphylococcal species, S. saprophyticus rarely causes hospital-acquired infections. Infections tend to be mild and responsive to first-line oral antibiotics, with a low risk of complications.
Rare but Significant Bacterial Causes
Although less frequently encountered, several other bacteria can cause UTIs, particularly in hospital settings or immunocompromised individuals.
Citrobacter spp.
These bacteria occasionally cause catheter-associated and nosocomial UTIs. They exhibit resistance to multiple antibiotics and are associated with opportunistic infections.
Serratia marcescens
Known for its distinctive red pigment, Serratia is an opportunistic pathogen that thrives in moist environments like hospital sinks and catheters, leading to outbreaks of hospital-acquired UTIs.
Morganella morganii
A urease-producing, Gram-negative bacterium, Morganella can cause complicated UTIs, particularly in patients with indwelling devices or structural urinary tract abnormalities.
Diagnosing Bacterial Urinary Tract Infections
Accurate and timely diagnosis of UTIs is crucial for effective treatment and the prevention of long-term complications. Diagnosis typically relies on a combination of clinical symptoms and laboratory tests.
Identifying the causative bacteria is particularly important in recurrent, complicated, or drug-resistant cases, where empirical treatment may fail.
Urinalysis
A rapid, simple screening tool, urinalysis detects the presence of leukocytes, nitrites, red blood cells, and bacteria in the urine, suggesting infection. It often serves as a first-line diagnostic approach in outpatient and emergency settings.
Urine Culture and Sensitivity Testing
This gold standard test involves culturing a urine sample to identify the causative bacteria and determine its antibiotic susceptibility. It guides precise therapy, especially in drug-resistant or recurrent infections.
Advanced Molecular Diagnostics
Polymerase Chain Reaction (PCR) and nucleic acid amplification techniques (NAATs) can rapidly detect bacterial DNA in urine samples. These modern methods offer enhanced sensitivity and faster turnaround times compared to traditional cultures.
Antibiotic Treatments for Bacterial UTIs
Antibiotics remain the cornerstone of UTI treatment. However, increasing antimicrobial resistance has made careful antibiotic selection and stewardship essential.
Treatment protocols depend on whether the UTI is uncomplicated, recurrent, or complicated by structural abnormalities or multidrug-resistant pathogens.
First-Line Medications
For uncomplicated UTIs, recommended first-line antibiotics include nitrofurantoin, fosfomycin, and trimethoprim-sulfamethoxazole. These agents effectively eradicate most uropathogens with minimal side effects.
Management of Drug-Resistant Infections
When faced with multidrug-resistant organisms, clinicians may turn to carbapenems, aminoglycosides, or combination therapies. Culture-based sensitivity testing ensures optimal antibiotic selection in such cases.
Natural and Alternative Remedies
Complementary therapies, such as cranberry extract, probiotics, and increased water intake, can help prevent UTI recurrences in at-risk individuals, although their efficacy varies.
Prevention of Bacterial Urinary Tract Infections
Prevention strategies are key to reducing the incidence of UTIs and their associated health complications. They encompass both personal hygiene measures and medical interventions.
Preventive measures are particularly important for individuals prone to recurrent infections, the elderly, and patients using indwelling catheters.
Personal Hygiene and Lifestyle Habits
Maintaining good genital hygiene, wiping front to back, urinating after intercourse, and staying well-hydrated significantly lowers UTI risk. Avoiding irritants such as harsh soaps and bubble baths also helps protect the urinary tract.
Medical Interventions and Prophylaxis
In high-risk individuals, prophylactic antibiotics or estrogen-based therapies (in postmenopausal women) are sometimes prescribed. Regular catheter replacement and use of antimicrobial-coated devices reduce catheter-associated UTI rates.
Complications from Untreated Urinary Tract Infections
If not diagnosed and treated in time, UTIs can lead to serious, potentially life-threatening complications. The severity of these outcomes depends on the infection’s site and duration.
Patients with comorbid conditions like diabetes or immunosuppression are at higher risk of developing these complications.
Sepsis
A severe systemic inflammatory response to infection, sepsis can result from untreated upper tract infections. It demands urgent medical attention to prevent organ failure and death.
Chronic Kidney Disease
Recurrent or untreated pyelonephritis can lead to renal scarring, reducing kidney function over time. This increases the risk of chronic kidney disease and hypertension.
Bladder Damage
Chronic inflammation and infection of the bladder may cause tissue damage, reduced bladder capacity, and long-term dysfunction, affecting urinary control.
Current Trends in UTI Research
Modern research is focusing on overcoming challenges posed by rising antimicrobial resistance and recurrent infections. Innovative therapies and preventive approaches are under development.
Collaborative global efforts also aim to improve UTI management through real-time surveillance and advanced molecular diagnostic tools.
Vaccine Development
Several experimental vaccines target E. coli adhesins, aiming to prevent initial bacterial attachment to the urinary epithelium. Clinical trials are ongoing to evaluate their efficacy.
Probiotic Therapies
Probiotics containing Lactobacillus species have shown promise in reducing UTI recurrence by restoring healthy vaginal and urinary flora and inhibiting pathogenic colonization.
Antimicrobial Resistance Monitoring
Global health agencies now track antimicrobial resistance patterns in UTI-causing bacteria. This information guides empirical treatment choices and infection control policies.
Conclusion
Urinary tract infections continue to represent a significant clinical challenge worldwide, particularly in women and hospitalized patients. E. coli remains the most frequent causative agent, but several other bacteria play critical roles in complicated and hospital-acquired infections.
Prompt and accurate diagnosis, tailored antibiotic treatment, and preventive measures are essential for reducing UTI-related morbidity and healthcare costs. Ongoing research into vaccines, probiotics, and resistance monitoring promises a more effective and sustainable approach to UTI management in the future.
Frequently Asked Questions (FAQ)
Which bacteria is the most common cause of UTIs?
Escherichia coli (E. coli) is responsible for 80–85% of all UTIs worldwide.
Can UTIs be sexually transmitted?
UTIs are not sexually transmitted, but sexual activity can increase the risk of bacterial entry into the urinary tract.
How are drug-resistant UTIs treated?
Drug-resistant UTIs require culture-guided antibiotic selection, often involving carbapenems, aminoglycosides, or combination therapies.
Related Contents
Columbia Agar with 5% Sheep Blood- Composition, Principle, Preparation, Results, Uses