In the field of clinical microbiology, the ability to rapidly and accurately identify bacterial pathogens is critical for patient care and infection control. Among these, Staphylococcus aureus remains a major cause of hospital- and community-acquired infections worldwide, often associated with severe complications.
One of the most reliable methods for differentiating Staphylococcus aureus from other staphylococcal species is the Coagulase Test. This article explores its principle, methodology, interpretations, and clinical significance in modern diagnostics.
Table of Contents
Importance of Identifying Staphylococcus aureus in Clinical Microbiology
Staphylococcus aureus is known for causing a range of conditions, from mild skin infections to life-threatening diseases like sepsis, endocarditis, and pneumonia. Its identification is essential, especially in hospital environments where methicillin-resistant Staphylococcus aureus (MRSA) strains pose a serious health threat.
Differentiating S. aureus from coagulase-negative staphylococci (CoNS) enables targeted treatment and effective infection control measures, reducing patient morbidity and healthcare costs.
Brief Overview of the Coagulase Test’s Diagnostic Role
The Coagulase Test plays a pivotal role in clinical microbiology laboratories for identifying S. aureus based on its ability to produce the coagulase enzyme. It remains a simple, rapid, and dependable method, forming a standard part of diagnostic protocols alongside modern molecular tests.
What is the Coagulase Test?
The Coagulase Test is a biochemical assay used to detect the presence of the enzyme coagulase produced by Staphylococcus aureus. This enzyme enables the bacterium to clot plasma by converting fibrinogen to fibrin.
The test is fundamental for confirming the identity of S. aureus isolates from clinical specimens such as pus, blood, and respiratory secretions, facilitating timely and appropriate therapeutic interventions.
Definition of Coagulase
Coagulase is an extracellular or bound enzyme produced primarily by Staphylococcus aureus. It interacts with plasma components, specifically prothrombin, forming a complex that converts soluble fibrinogen into insoluble fibrin, resulting in clot formation.
The presence of this enzyme is a distinctive biochemical marker used to separate S. aureus from other staphylococcal species, which lack coagulase activity.
Purpose and Importance of the Test in Microbiology
The Coagulase Test provides a rapid means to differentiate pathogenic S. aureus from less virulent coagulase-negative staphylococci (CoNS). This distinction is crucial because S. aureus infections often require aggressive antimicrobial therapy and heightened infection control measures.
Additionally, coagulase detection is useful for monitoring hospital-acquired infection outbreaks and for epidemiological surveillance of antibiotic-resistant strains like MRSA.
Principle of the Coagulase Test
The principle of the Coagulase Test relies on the ability of coagulase produced by S. aureus to react with plasma and form fibrin clots. This clotting can be observed macroscopically as visible clumps or a firm clot in a test tube.
This reaction can be demonstrated using either a slide test for bound coagulase (clumping factor) or a tube test for free coagulase, providing reliable identification of the organism.
How Coagulase Enzyme Works
Coagulase acts as a virulence factor by enabling S. aureus to evade host immune defenses. It binds to prothrombin to form a staphylothrombin complex, which converts fibrinogen to fibrin, thereby clotting plasma.
This clot can surround bacterial cells, protecting them from phagocytosis and other immune responses, contributing to the pathogenicity of S. aureus.
Mechanism of Plasma Clot Formation
During the test, when plasma containing fibrinogen encounters coagulase, the enzyme activates prothrombin. The activated complex converts fibrinogen into fibrin threads, which entangle bacterial cells and plasma proteins to form a visible clot.
The presence or absence of clotting in the reaction mixture serves as a clear indicator of coagulase activity and thus the presence of S. aureus.
Types of Coagulase Tests
To comprehensively detect coagulase production, several variations of the Coagulase Test are employed in clinical microbiology. Each type targets different forms of the enzyme — either bound to the bacterial cell wall or free in the extracellular environment.
The two most commonly used formats are the Slide Coagulase Test for detecting bound coagulase (clumping factor) and the Tube Coagulase Test for detecting free coagulase. Additionally, rapid immunological tests like latex agglutination have been developed for faster results.
Slide Coagulase Test
The Slide Coagulase Test is a quick, direct method for detecting bound coagulase present on the surface of Staphylococcus aureus. It is frequently used for preliminary screening in clinical labs due to its simplicity and speed.
Principle
This test works on the principle that bound coagulase, or clumping factor, directly reacts with fibrinogen in plasma, causing visible clumping (agglutination) on a glass slide.
Procedure
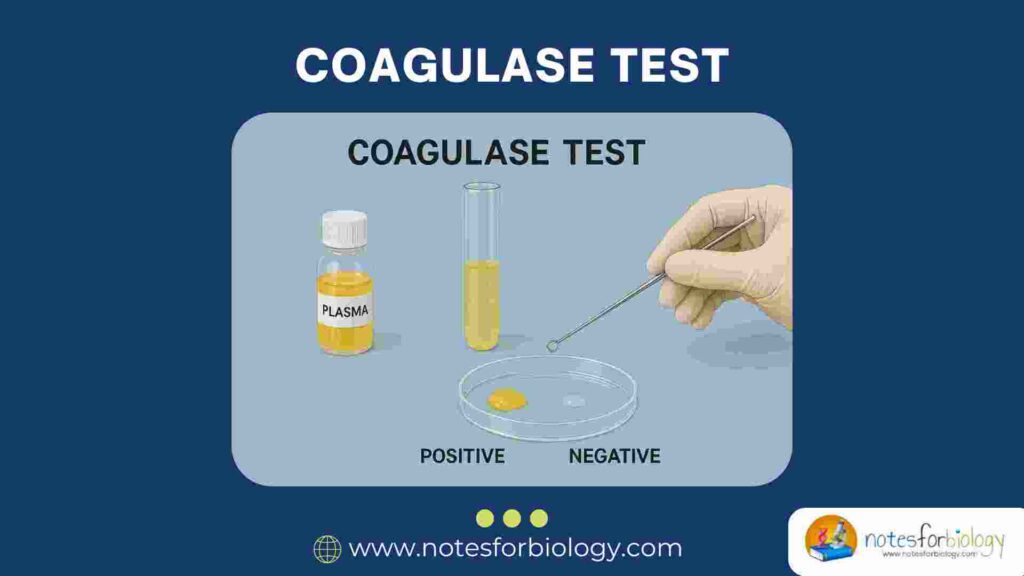
A clean, dry glass slide is divided into two sections — one for the test organism and one for control. A drop of plasma is mixed with a bacterial suspension on one section, while the other section contains plasma and sterile saline. Immediate clumping indicates a positive result.
Interpretation
Visible clumping within 10 seconds confirms the presence of bound coagulase and identifies the organism as Staphylococcus aureus. The control section ensures that clumping isn’t due to auto-agglutination or contaminants.
Tube Coagulase Test
The Tube Coagulase Test detects free coagulase secreted by S. aureus into the surrounding environment. It is considered the definitive method for confirming coagulase activity.
Principle
In this method, the free coagulase reacts with coagulase-reacting factor (CRF) present in plasma, forming a complex that converts fibrinogen into a fibrin clot.
Procedure
A suspension of the test organism is prepared in plasma and incubated at 37°C. The tube is observed at intervals up to 24 hours for the formation of a clot, which may range from a loose clot to a firm, immovable one.
Interpretation
The formation of a clot indicates a positive result, confirming the presence of free coagulase and identifying the organism as S. aureus. Lack of clot formation after 24 hours is considered a negative result.
Other Variants (e.g., Latex Agglutination Test)
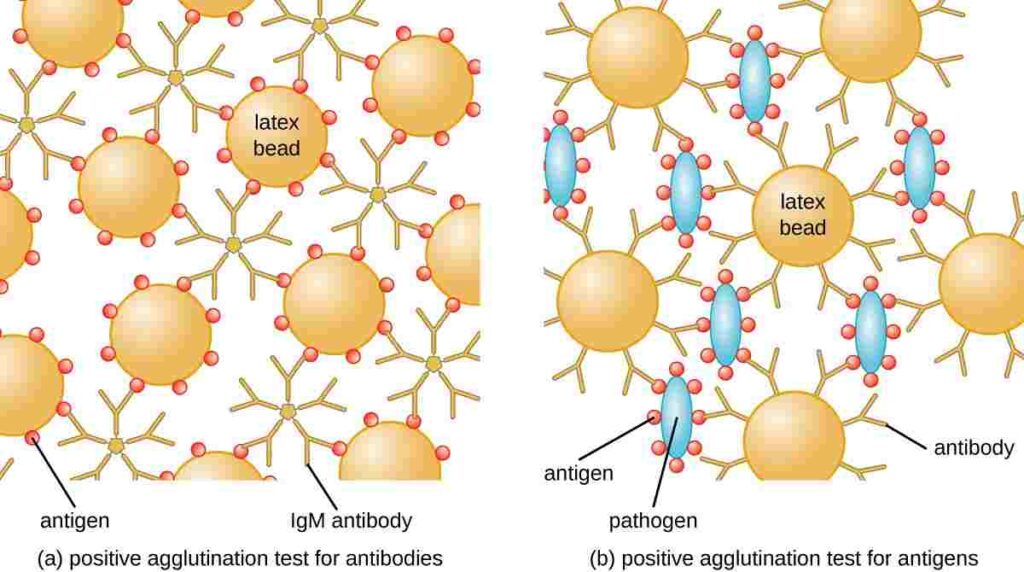
Modern diagnostic laboratories increasingly use latex agglutination tests, where latex particles coated with fibrinogen and IgG react with both bound coagulase and protein A of S. aureus. Agglutination within minutes confirms the organism’s identity, offering a rapid and reliable alternative to traditional methods.
Step-by-Step Procedure of Coagulase Tests
Accurate coagulase testing requires careful preparation of materials, plasma, and bacterial suspensions, along with strict adherence to protocols to prevent errors and false readings.
Materials Required
Basic materials include sterile glass slides, test tubes, inoculating loops, incubators, human or rabbit plasma (free of anticoagulants like EDTA), sterile saline, and bacterial cultures grown on nutrient-rich media.
Plasma Source and Preparation
Freshly collected rabbit plasma is commonly used, though human plasma can also be employed. Plasma should be free from fibrin clots and anticoagulants that may interfere with test accuracy. It must be stored properly and brought to room temperature before use.
Test Organism Preparation
The test organism is typically cultured overnight on nutrient agar or blood agar plates. A dense bacterial suspension is made using sterile saline or broth to ensure an adequate concentration for reliable test results.
Detailed Slide Test Protocol
- Place a drop of plasma and sterile saline on a clean glass slide.
- Emulsify a portion of the test colony into both drops.
- Gently rock the slide and observe for clumping within 10 seconds.
- Include known positive and negative control strains for comparison.
Detailed Tube Test Protocol
- Inoculate 0.5 mL of plasma with a loopful of the test organism in a sterile test tube.
- Incubate at 37°C.
- Examine for clot formation at 1, 2, 4, and 24 hours.
- If no clot is present after 24 hours, the result is considered negative.
Interpretation of Results
Correct interpretation ensures accurate identification of Staphylococcus aureus and prevents diagnostic errors.
Positive and Negative Results
- Positive Result: Immediate clumping in the slide test or clot formation in the tube test indicates coagulase production and confirms the presence of S. aureus.
- Negative Result: Absence of clumping or clot after specified times indicates a coagulase-negative staphylococcal species (CoNS).
Factors Affecting Test Accuracy
Factors such as the quality and freshness of plasma, proper incubation temperature, bacterial concentration, and avoiding plasma contamination are vital for reliable outcomes.
Quality Control in Coagulase Testing
Laboratory best practices require the use of positive and negative control strains in every batch of testing to validate results and prevent misidentification.
Use of Control Strains
A known S. aureus strain is used as a positive control, while a coagulase-negative Staphylococcus epidermidis strain serves as a negative control, ensuring the test system functions correctly.
Troubleshooting Common Errors
Common issues include auto-agglutination, deteriorated plasma, or improper incubation. Correcting these problems involves using fresh reagents, confirming control results, and adhering to protocols meticulously.
Clinical Significance and Applications
The Coagulase Test holds considerable importance in medical microbiology due to its diagnostic value in infection control and antimicrobial stewardship programs.
Differentiating Staphylococcus aureus from Coagulase-Negative Staphylococci
This test remains the most efficient way to distinguish S. aureus from CoNS, which are often skin commensals but can cause opportunistic infections in immunocompromised individuals or patients with prosthetic devices.
Importance in Hospital-Acquired Infections
Prompt identification of S. aureus is crucial for managing hospital-acquired infections (HAIs) like surgical site infections, bloodstream infections, and ventilator-associated pneumonia. Timely diagnosis enables appropriate antibiotic therapy and isolation precautions.
Role in Antimicrobial Resistance Screening
Since many MRSA strains retain coagulase activity, the test aids in rapid MRSA screening when combined with methicillin susceptibility tests, guiding treatment decisions and infection control measures.
Limitations of the Coagulase Test
Although highly reliable, the Coagulase Test has certain limitations and should not be used as the sole diagnostic criterion.
False Positive and False Negative Scenarios
Auto-agglutination by some staphylococcal strains may produce false-positive slide test results. Prolonged incubation or contaminated plasma can cause false-negative tube test results. Complementary tests help resolve discrepancies.
Need for Complementary Diagnostic Tests
Additional tests such as mannitol fermentation, DNase testing, and molecular assays are often performed alongside the Coagulase Test to confirm S. aureus identity and detect methicillin resistance genes like mecA.
Recent Advances in Coagulase Testing
Modern microbiology has introduced several innovations that enhance the speed, accuracy, and reliability of coagulase detection in clinical specimens.
Automated Coagulase Test Systems
Automated blood culture systems now incorporate coagulase testing modules that detect clot formation or agglutination electronically, reducing labor and result turnaround times.
Molecular and Rapid Immunological Methods
Rapid immunological techniques, such as latex agglutination kits and PCR assays targeting the coagulase gene, offer quick, specific, and sensitive detection of S. aureus, proving valuable in critical care and outbreak settings.
Safety and Biosafety Precautions
Handling human or animal plasma and bacterial cultures poses biohazard risks. Strict adherence to biosafety practices ensures laboratory personnel safety and prevents contamination.
Handling Human Plasma
Human-derived plasma should be screened for blood-borne pathogens and handled using appropriate personal protective equipment (PPE) like gloves, lab coats, and eye protection.
Disposal of Infectious Material
All biological waste, including plasma and bacterial suspensions, must be autoclaved or disposed of in biohazard containers to prevent accidental exposure and environmental contamination.
Conclusion
The Coagulase Test remains a cornerstone in clinical microbiology for the identification of Staphylococcus aureus. Its simplicity, reliability, and diagnostic significance continue to make it indispensable despite the availability of modern molecular techniques.
As the global threat of antimicrobial resistance grows, rapid and accurate identification of S. aureus through coagulase testing plays a critical role in patient management, infection control, and public health protection.
Frequently Asked Questions (FAQ)
What are the two main types of Coagulase Tests?
The two main types are the Slide Coagulase Test (detects bound coagulase or clumping factor) and the Tube Coagulase Test (detects free coagulase in plasma).
How is a positive Coagulase Test confirmed?
A positive result is confirmed by visible clumping in the slide test or fibrin clot formation in the tube test, along with appropriate positive and negative control results.
Why is Staphylococcus aureus coagulase-positive?
Staphylococcus aureus produces the coagulase enzyme as a virulence factor, allowing it to clot plasma and evade host immune defenses by forming protective fibrin barriers around itself.
Related Contents
Clostridium perfringens: Overview, Enterotoxins and Food Poisoning
CLED Agar- Composition, Principle, Preparation, Results, Uses